Videos
Browse videos by topic
All Videos
Showing 217-240 of 345 videos

VEEVA VAULT Online Training Explained By Expert: Everything You Need to Know
MaxMunus Training
/@maxmunustraining
Apr 19, 2022
This video provides an overview of Veeva Vault training, highlighting its importance as a cloud-based enterprise content management platform specifically designed for the biological sciences. It emphasizes Veeva Vault's role in providing a single source of truth for content and data, thereby minimizing complexity and enhancing business agility within life sciences organizations. The training covers a comprehensive range of topics, from basic end-user functions like document and binder management to advanced administrative operations such as configuring document types, workflows, and dynamic access controls. The video also details Veeva's certification programs and underscores the significant global job opportunities available for Veeva Vault professionals, citing major pharmaceutical and life sciences companies as key employers. Key Takeaways: * **Veeva Vault as a Core Life Sciences Platform:** Veeva Vault is presented as an indispensable cloud enterprise content management platform for biological sciences, crucial for streamlining regulatory processes, data management, and ensuring compliance by providing a unified source of truth. * **Comprehensive Functional Scope:** The training curriculum covers a wide array of Veeva Vault functionalities, from fundamental document and binder operations to intricate system administration, including document type hierarchies, workflow creation, and dynamic access control, indicating its deep capabilities for managing complex industry content. * **High Market Demand for Expertise:** There is a robust global job market for Veeva Vault professionals across various roles (e.g., Veeva Vault Lead, Senior Manager Veeva CRM, Analyst, Developer), with significant opportunities in major pharmaceutical and biotech companies, highlighting the value of this specialized skill set. * **Integration within the Veeva Ecosystem:** The mention of "Veeva Products Overview" and "Veeva CRM Certified White Belt qualification" suggests that Veeva Vault is an integral part of a broader Veeva suite, implying that expertise in Vault is complementary to other Veeva solutions like CRM. * **Focus on Implementation and Configuration:** The training emphasizes "implementation and configuration level" learning, indicating a practical, hands-on approach designed to make participants "project ready" and capable of deploying and managing Veeva Vault effectively from day one. * **Regulatory Compliance and Data Integrity:** The platform's design for "biological sciences" to "minimize complexity" and serve as a "unique source of truth" directly addresses critical industry needs for regulatory compliance, data integrity, and efficient information governance, aligning with stringent industry standards.

Patient Must Come First in Value Based Care
AHealthcareZ - Healthcare Finance Explained
@ahealthcarez
Apr 16, 2022
This video provides an in-depth exploration of Value-Based Care (VBC) and the critical, often overlooked, imperative to prioritize the patient within this evolving healthcare model. Dr. Eric Bricker of AHealthcareZ discusses an article by Dr. Sachin Jain, CEO of SCAN Health, a non-profit Medicare Advantage plan, who brings extensive experience from government, major carriers, and direct patient care. The video establishes that while VBC is frequently praised in theory, its practical implementation often reverts to cost-containment strategies reminiscent of past managed care models, potentially sidelining patient well-being. The core of the discussion revolves around Michael Porter's value equation—quality divided by cost—and how VBC aims to increase quality while decreasing cost. However, Dr. Jain's enumerated seven tenets of VBC reveal a more complex reality. These tenets include stringent management of inpatient bed-days, mandatory specialist referrals requiring prior authorization, the use of narrow networks that may prioritize cost over specialist quality, and team-based care that can introduce additional gatekeepers before a patient sees a physician. Furthermore, VBC often involves low-cost formularies that limit access to newer, potentially expensive medications, an emphasis on addressing social determinants of health (though without robust population-level evidence of effectiveness), and ultimately, a focus on the VBC plan's own revenue and bottom line. Dr. Bricker highlights the striking similarities between these VBC tenets and the much-criticized HMO models of the 1990s, which faced significant backlash for failing to put patients first. To counteract this tendency and genuinely embed patient-centricity into VBC, Dr. Bricker proposes three structural and incentive-based solutions. These include placing physicians on salary with transparent variable compensation to remove financial incentives for delivering more or less care, establishing a third-party ombudsman or rapid response team (RRT) hotline for patients and healthcare staff to report issues of denied care or bureaucratic hurdles, and mandating that all professionals involved in designing or administering VBC plans (from doctors to politicians) must themselves be enrolled in a VBC insurance plan. These suggestions emphasize transparency and accountability, drawing parallels to the "sunlight is the best disinfectant" principle and Toyota's quality improvement process where any assembly line worker can halt production to address a problem. Key Takeaways: * **Value-Based Care (VBC) Definition:** VBC is theoretically defined by the value equation: Quality divided by Cost. The goal is to improve patient outcomes (quality) while reducing healthcare expenditures (cost). * **Practical Tenets of VBC:** Dr. Sachin Jain outlines seven practical tenets of VBC, which often prioritize cost control: managing inpatient bed-days, requiring specialist referrals, utilizing narrow networks, implementing team-based care, employing low-cost formularies, addressing social determinants of health, and focusing on the VBC plan's revenue. * **Cost Containment Strategies:** VBC models often involve aggressive strategies to reduce costs, such as minimizing hospital stays, requiring prior authorizations for specialist visits, and restricting choices of providers through narrow networks, which can sometimes override quality considerations. * **Gatekeeping in Care Delivery:** Team-based care, while beneficial in some aspects, can also create additional layers of gatekeepers (e.g., nurse practitioners before PCPs, PCPs before specialists), potentially delaying or complicating patient access to specialized care. * **Impact on Pharmaceutical Access:** Low-cost formularies are a critical component of VBC, limiting patient access to newer, often more expensive, medications. This directly impacts pharmaceutical companies' market access strategies and patient treatment options. * **Social Determinants of Health (SDOH):** While addressing SDOH is a VBC tenet, the video notes a lack of population-level studies proving its effectiveness, though individual cases (like providing a refrigerator for insulin storage) demonstrate its potential impact. * **Historical Parallels to HMOs:** The speaker draws a strong comparison between the current practical implementation of VBC and the much-criticized Health Maintenance Organizations (HMOs) of the 1990s, which faced backlash for not prioritizing patients. * **Ethical Imperative of Patient-First:** The fundamental ethical principle of "the patient comes first," ingrained in medical education, must serve as the guiding framework for all VBC strategies to prevent a repeat of past managed care failures. * **Physician Compensation Reform:** A proposed solution involves putting physicians on salary with transparent variable compensation. This aims to remove financial incentives that might lead doctors to provide either too much or too little care, allowing clinical judgment to be paramount. * **Third-Party Ombudsman for Accountability:** Implementing a third-party ombudsman or a "rapid response team" (RRT) hotline allows patients, doctors, and other healthcare team members to report issues like denied care, bureaucratic hurdles, or lack of access, fostering transparency and external scrutiny. * **"Eat Your Own Cooking" Principle:** A key recommendation is that all individuals involved in designing, administering, or regulating VBC (including doctors, administrators, insurance employees, and government officials) should be enrolled in VBC insurance plans themselves. This ensures they experience the system firsthand and are incentivized to create a patient-centric model. * **Transparency as a Disinfectant:** The overarching theme for proposed solutions is transparency, echoing Louis Brandeis's sentiment that "sunlight is the best disinfectant." Openness about compensation structures and avenues for reporting issues can drive accountability and patient-centricity. Key Concepts: * **Value-Based Care (VBC):** A healthcare delivery model where providers are paid based on patient health outcomes, rather than the volume of services provided. * **Value Equation (Quality / Cost):** A framework, popularized by Michael Porter, for defining value in healthcare as the health outcomes achieved per dollar spent. * **Medicare Advantage Plan:** A type of Medicare health plan offered by a private company that contracts with Medicare to provide all your Part A and Part B benefits. * **Formulary:** A list of prescription drugs covered by a health insurance plan. "Low-cost formularies" typically prioritize generic or less expensive brand-name drugs. * **Narrow Network:** A health insurance plan that restricts patients to a limited number of doctors and hospitals, often to control costs. * **Social Determinants of Health (SDOH):** Non-medical factors that influence health outcomes, such as socioeconomic status, education, neighborhood and physical environment, employment, and social support networks. * **Rapid Response Team (RRT):** A team of healthcare professionals in hospitals who respond to patients whose condition is deteriorating, before a full cardiac arrest or respiratory failure occurs. The video suggests an outpatient version for VBC issues. * **Ombudsman:** An official appointed to investigate individuals' complaints against maladministration, especially that of public authorities. * **Fee-for-service:** A payment model where providers are paid for each service they perform (e.g., office visit, test, procedure). Examples/Case Studies: * **SCAN Health:** Dr. Sachin Jain's non-profit Medicare Advantage plan in Southern California, serving as a real-world example of a VBC organization. * **Diabetic Patient and Refrigerator:** An example of addressing a social determinant of health where Dr. Jain's health plan purchased a refrigerator for a diabetic patient to properly store insulin. * **1990s HMOs:** The video frequently references the historical backlash against HMOs in the 1990s due to their cost-cutting measures leading to patient dissatisfaction, drawing a parallel to current VBC practices. * **Toyota Quality Improvement Process:** The analogy of Toyota's "Andon cord" system, where any worker can stop the assembly line to address a quality issue, is used to illustrate the concept of a rapid response team or ombudsman in VBC.

eTMF System Specific Training (Veeva Vault)
Power of Work
/@powerofwork6914
Apr 13, 2022
This video provides specific training on the Veeva Vault eTMF (electronic Trial Master File) system, focusing on its features and functionalities for managing clinical trial documentation within the life sciences industry. The speaker, from Power of Work, guides viewers through navigating the system, applying filters, viewing documents, and critically, generating reports. The discussion highlights the transition from paper-based TMFs to eTMFs, emphasizing the significant advantages Veeva Vault offers in terms of regulatory compliance, data visibility, collaboration, and security. It also touches upon the system's role in supporting TMF specialists and its broader integration within the Veeva ecosystem. Key Takeaways: * **Veeva Vault as a Prevalent eTMF Solution:** Veeva Vault is presented as a widely adopted, comprehensive, cloud-based eTMF platform, particularly suited for large pharmaceutical companies due to its extensive features and the robust IT support required for its maintenance and updates. * **Ensuring Regulatory Compliance:** The video underscores the critical role of eTMF systems like Veeva Vault in maintaining regulatory compliance, specifically mentioning 21 CFR Part 11, electronic signatures, and audit trails. It emphasizes that a complete and accurate TMF is essential for successful FDA and other regulatory agency inspections. * **Enhanced Data Visibility and Reporting Capabilities:** Veeva Vault significantly improves operational efficiency by offering advanced filtering and reporting functions. These allow users to gain real-time insights into TMF completeness, track document processing, and monitor team performance, which is crucial for proactive management and audit readiness. * **Secure Collaboration and Audit Trails:** The system facilitates secure external collaboration, enabling multiple stakeholders to access and contribute to the TMF with defined roles and permissions. Its robust audit trail functionality ensures accountability and traceability for all document interactions, enhancing data integrity. * **Strategic Importance of Metadata Management:** The training highlights that a key aspect of TMF quality control involves cross-referencing document content with its associated metadata within the system, stressing the necessity for accurate data entry and consistency for effective document retrieval and reporting. * **Integration within the Life Sciences Technology Landscape:** The video notes Veeva Vault's evolving integration capabilities, including its use as a Clinical Trial Management System (CTMS), indicating its broader role and interconnectedness within the suite of technology solutions utilized in clinical research.

High Cost Healthcare Claimants
AHealthcareZ - Healthcare Finance Explained
@ahealthcarez
Apr 10, 2022
This video provides an in-depth exploration of the primary driver of high healthcare costs in employer-sponsored health plans: high-cost claimants. Dr. Eric Bricker, the speaker, begins by establishing the context that anyone involved in managing a health plan budget must constantly focus on these individuals. He highlights the well-known 80/20 rule, where 80% of healthcare costs are driven by just 20% of claimants (typically those exceeding $25,000 annually), and further emphasizes the 5/50 rule, where 50% of costs come from the top 5% of claimants (those over $100,000 per year). The core message is that addressing overall healthcare costs is impossible without directly confronting the issue of high-cost claimants. The presentation then delves into categorizing high-cost claimants, first by their primary diagnostic areas and then by their claims patterns. Dr. Bricker identifies three major diagnostic categories: musculoskeletal (MSK), cardiovascular, and cancer. He provides important nuances, such as including "injury and poisoning" within MSK for a more accurate spend analysis, and expanding "cardiovascular" to encompass diabetes and renal failure, as these often stem from the same underlying vascular pathologies. He stresses that daily attention to these three categories is crucial for effective cost management. Following the diagnostic breakdown, the video introduces a critical framework for understanding the heterogeneity of high-cost claimants, noting that two-thirds of them are new each year. Dr. Bricker outlines three distinct claims patterns: "The Explosion," representing about 50% of new high-cost claimants, characterized by sudden, catastrophic events with little to no prior claims (e.g., heart attack, stroke, new cancer diagnosis); "The Ramp-Up," accounting for approximately 17% of high-cost claimants, showing a gradual increase in costs over time (e.g., progression to dialysis for end-stage renal disease); and "The Continuation," making up about 33% of high-cost claimants, who were high-cost in the previous year and remain so (e.g., cancer recurrence, congestive heart failure, complex surgical complications). He concludes by discussing the three ways claimants exit the high-cost category: leaving the plan, expiring, or resolving their condition. Key Takeaways: • **High-Cost Claimants Drive the Majority of Healthcare Costs:** A disproportionate amount of healthcare spend is concentrated in a small percentage of claimants. Specifically, 80% of costs are driven by 20% of claimants (typically >$25K/year), and 50% by just 5% of claimants (typically >$100K/year). This concentration necessitates a focused strategy. • **Primary Diagnostic Categories:** The vast majority of high-cost claims fall into three main diagnostic areas: Musculoskeletal (MSK), Cardiovascular, and Cancer. Employers and benefits managers must prioritize understanding and addressing these specific health challenges. • **MSK Spend Includes Injury:** When analyzing musculoskeletal costs, it's crucial to include "injury and poisoning" diagnostic codes, as many long-term musculoskeletal issues are categorized under injury, which can be overlooked if only "MSK" codes are considered. • **Cardiovascular Spend Encompasses Diabetes and Renal Failure:** Cardiovascular costs extend beyond direct heart and stroke events to include diabetes and kidney failure. These conditions share common vascular damage pathologies, making their management integral to a comprehensive cardiovascular health strategy. • **Three Distinct Claims Patterns:** High-cost claimants are not a homogeneous group but follow three patterns: "The Explosion" (sudden, catastrophic events with no prior claims, ~50% of new high-cost claimants), "The Ramp-Up" (gradual increase in costs over time, ~17%), and "The Continuation" (ongoing high costs from previous years, ~33%). • **Challenges in Predicting "The Explosion":** Claims analytics are ineffective for "Explosion" type claimants because they have no prior claims data to analyze. This highlights a significant limitation of retrospective data analysis for a large segment of high-cost events. • **Primary Care as a Solution for "The Explosion":** For "Explosion" claimants, the most effective intervention is robust primary care. This can be delivered through various models (onsite, nearsite, direct primary care, virtual) and is essential for early detection and prevention before catastrophic events occur. • **Proactive Intervention for "The Ramp-Up":** Claims analytics are highly effective for identifying "Ramp-Up" claimants, such as those progressing towards renal failure due to diabetes or hypertension. Employers should aim for 100% identification of these individuals to enable timely and impactful interventions. • **Ongoing Management for "The Continuation":** Claimants in "The Continuation" category require sustained management and support due to chronic or recurring conditions like cancer recurrence, congestive heart failure, or complications from previous surgeries. • **Two-Thirds of High-Cost Claimants are New Annually:** The majority of high-cost claimants (two-thirds) are new each year, meaning strategies cannot solely focus on existing high-cost individuals but must also account for continuous new entries. • **Cut Through Distractions:** Benefits managers, HR, and CFOs must resist getting sidetracked by numerous health plan distractions (plan design, compliance, employee complaints, data issues) and maintain a daily focus on addressing high-cost claimants. • **Claimant Exit Strategies:** High-cost claimants exit the category through three main avenues: leaving the health plan (e.g., employee changes jobs), expiring, or resolving their medical condition (e.g., successful cancer treatment, kidney transplant). Key Concepts: * **High Cost Claimants:** Individuals whose healthcare claims exceed a specific annual financial threshold (e.g., $25,000 or $100,000), accounting for a disproportionately large share of total healthcare expenditures. * **80/20 Rule (Pareto Principle):** A general rule stating that roughly 80% of effects come from 20% of causes. In healthcare, this means 80% of costs are driven by 20% of claimants. * **5/50 Rule:** A more extreme variant of the Pareto Principle, indicating that 50% of healthcare costs are driven by just 5% of claimants. * **Diagnostic Categories:** Broad medical classifications used to group similar conditions, which in this context, highlight the primary areas of high healthcare spend (MSK, Cardiovascular, Cancer). * **Claims Patterns:** Distinct trajectories of healthcare utilization and cost accumulation over time, categorized as "The Explosion," "The Ramp-Up," and "The Continuation." * **Primary Care:** Comprehensive, first-contact healthcare that focuses on prevention, early detection, and management of common health problems, crucial for mitigating "Explosion" type high-cost events. Examples/Case Studies: * **"The Explosion" Examples:** Heart attack, stroke, or a new cancer diagnosis in an otherwise healthy individual (e.g., a 45-year-old with metastatic colon cancer appearing suddenly). * **"The Ramp-Up" Examples:** The progressive decline of kidney function leading to dialysis for End-Stage Renal Disease, often secondary to long-standing diabetes and hypertension. * **"The Continuation" Examples:** Recurrence or metastasis of cancer, ongoing management of congestive heart failure, complications from unsuccessful spine surgery, or the need for revision surgeries for joint replacements.

eTMF Systems Introduction
Power of Work
/@powerofwork6914
Apr 1, 2022
This video provides a comprehensive introduction to eTMF (electronic Trial Master File) systems, detailing their evolution from paper-based documentation to digital platforms in clinical research. The speaker emphasizes the critical role of eTMFs in managing the extensive documentation generated during clinical trials, highlighting their importance for regulatory compliance, particularly during FDA audits. The content covers the historical context, the necessity for digital transformation due to increasing trial complexity, and the numerous advantages of eTMF systems, including enhanced document retrieval, real-time tracking, robust quality control processes, improved reporting, SOP compliance, cost savings, and seamless collaboration between sponsor companies and Contract Research Organizations (CROs). The video also touches upon specific eTMF systems, notably mentioning Veeva Vault, and discusses practical aspects of document management, metadata entry, and filing structures within these systems. * **Operational Efficiency and Data Integrity:** The digital nature of eTMFs significantly improves operational efficiency through features like real-time tracking, timestamping, and multi-step quality control, ensuring data integrity and reducing the risks associated with manual, paper-based processes. * **Data Management and Reporting Capabilities:** eTMF systems enable sophisticated data management through structured metadata and robust reporting tools, allowing for better organization, retrieval, and analysis of clinical trial documents * **Addressing Industry Skill Gaps:** The video highlights a significant industry demand for professionals with technical eTMF system skills combined with clinical research knowledge, indicating a potential market for specialized consulting, training, or AI-powered assistance for these roles. * **Facilitating Collaboration in Clinical Ecosystems:** eTMFs are crucial for fostering efficient collaboration among diverse stakeholders in clinical trials, including sponsors, CROs, and sites, by providing controlled, shared access to critical documentation.

Healthcare IT Interoperability and EMR Interoperability Explained
AHealthcareZ - Healthcare Finance Explained
@ahealthcarez
Mar 27, 2022
This video provides an in-depth exploration of Electronic Medical Record (EMR) and Electronic Health Record (EHR) interoperability, focusing on the challenges and realities of sharing healthcare data between different hospital systems and doctor practices in the United States. Dr. Eric Bricker begins by establishing the context that the vast majority of health information is now stored electronically, moving away from traditional paper charts. He highlights the historical problem of data siloing, where individual healthcare providers had their own computer systems that did not communicate, leading to fragmented patient information. The presentation then delves into the widespread consensus among various stakeholders—patients, federal and state governments, insurance companies, employers, and even the American Hospital Association (AHA)—that health information *should* be shared. The stated benefits of interoperability are compelling: increased patient safety, improved care quality, enhanced ability to track public health issues like pandemics, and decreased healthcare costs. Despite this universal agreement on the desirability of data sharing, Dr. Bricker transitions to reveal the stark reality of its implementation across major U.S. cities, citing data from the federal government. The video presents specific statistics on the percentage of hospitals sharing patient data in various metropolitan areas, showcasing a wide disparity: Cleveland leads at 78%, followed by Miami (77%) and Dallas (60%), while Boston stands at 50%, and Philadelphia lags significantly at only 35%. Dr. Bricker expresses skepticism and disappointment at these low figures, questioning why such fundamental data sharing remains elusive in an advanced technological era. He then introduces a critical insight: the barriers to interoperability are not solely technological. He shares a compelling true story about a large multi-specialty physician practice (over 500 doctors) that *deliberately* stopped sharing CT images with a local hospital, despite having previously seamless, cost-free interoperability. Instead, they began charging patients to burn images onto CDs, forcing patients to physically transport them. This policy change, he notes, correlated with the practice being acquired by a private equity firm, suggesting that financial incentives and strategic patient retention (using data as leverage) can override patient-centered care and efficient data sharing. Key Takeaways: * **Definition of EMR/EHR Interoperability:** Interoperability refers to the ability of different healthcare systems and practices to seamlessly share electronic patient data, including disease history, physical exam findings, lab results, and imaging scans (CT, MRI, X-rays). * **Universal Desire for Data Sharing:** There is broad consensus across patients, federal and state governments, insurance companies, employers, and even the American Hospital Association (AHA) that health information should be shared for better healthcare coordination. * **Significant Benefits of Interoperability:** Sharing health data is crucial for increasing patient safety, improving care quality, facilitating the tracking and management of public health crises like pandemics, and ultimately decreasing overall healthcare costs. * **Low Rates of Actual Interoperability:** Despite the recognized benefits and technological capabilities, the actual rates of health information sharing among hospitals in major U.S. cities remain surprisingly low, with figures ranging from a high of 78% in Cleveland to a mere 35% in Philadelphia. * **Beyond Technological Barriers:** The primary obstacles to interoperability are often not technological limitations but rather organizational unwillingness, competitive strategies, and financial incentives that prioritize self-interest over patient care. * **Data as a Competitive Lever:** Healthcare providers, particularly large physician practices and hospital systems, may intentionally restrict data sharing to increase "patient stickiness," making it harder for patients to seek care elsewhere and reducing competition based on price and quality. * **Impact of Private Equity Ownership:** A real-world case study illustrates how a multi-specialty practice, after being acquired by a private equity firm, ceased providing direct access to patient imaging data to an affiliated hospital, instead reverting to cumbersome, patient-burdened methods like burning CDs. * **Discrepancy Between Stated and Actual Priorities:** Organizations often claim to be "patient-centered" in their marketing, but their actions, such as deliberately hindering data sharing, reveal their true priorities, which may be profit or market control. * **Inefficiency of Non-Interoperable Data Transfer:** The practice of burning medical images onto CDs for patient transport is highlighted as an outdated, clunky, and inefficient process that significantly impedes timely and effective patient care, especially in critical situations like cancer diagnosis. * **Implications for Patient Choice and Quality of Care:** The lack of interoperability can restrict patients' access to world-expert physicians or alternative care settings, as their data is held captive within specific health systems, potentially compromising optimal treatment outcomes. Key Concepts: * **EMR (Electronic Medical Record):** A digital version of a patient's chart from a single practice or hospital. * **EHR (Electronic Health Record):** A more comprehensive digital record of a patient's health information that is shareable across different healthcare settings. * **Interoperability:** The ability of different information systems, devices, and applications to access, exchange, integrate, and cooperatively use data in a coordinated manner. * **Data Siloing:** The isolation of data within individual systems or departments, preventing easy access and sharing across an organization or between different organizations. Examples/Case Studies: * **U.S. Government Interoperability Survey:** Data from the federal government (healthit.gov) on the percentage of hospitals sharing patient data in major U.S. cities, including Cleveland (78%), Miami (77%), Dallas (60%), New York City (59%), Chicago (58%), Boston (50%), Washington D.C. (44%), Los Angeles (41%), and Philadelphia (35%). * **Multi-Specialty Physician Practice Case Study:** A 500+ doctor multi-specialty practice in a major U.S. city that ceased providing direct electronic access to CT images for a local hospital, instead requiring patients to pay for and transport images on CDs, a policy change that correlated with new private equity ownership.

Top 10 Reasons to Podcast
Self-Funded
@SelfFunded
Mar 25, 2022
This video provides an in-depth exploration of the top ten reasons why individuals and businesses, particularly those in sales, should consider starting a podcast. The speaker, Spencer Smith, presents a compelling argument for podcasting as a powerful tool for business development, brand building, and lead generation, drawing from his personal experience with his "Self-Funded" podcast. He frames podcasting not merely as a content creation activity but as a strategic sales and marketing initiative that can significantly accelerate traditional business growth cycles. The presentation progresses through a structured list of ten benefits, starting with immediate brand recognition and moving through various stages of relationship building, credibility establishment, and ultimately, lead generation and content longevity. Smith emphasizes that a podcast allows the host to control the narrative, invite industry experts, and build a platform that positions them as a thought leader. He contrasts the traditional struggle to gain a "seat at the table" with the empowerment of creating one's own table, inviting high-profile guests, and shaping the discourse around relevant topics. A core theme throughout the discussion is the shift from transactional selling to value-driven engagement. Smith highlights that a podcast inherently sells value and ideas, offering free information and fostering trust without an immediate product pitch. This approach, he argues, builds rapport and credibility far more effectively and quickly than conventional sales methods. He illustrates how consistent content creation leads to a library of reusable assets that can serve as perpetual lead generation tools and follow-up resources, significantly reducing the manual effort typically required in the sales process. The speaker's perspective is highly practical and results-oriented, focusing on the tangible benefits for a salesperson or business owner. He shares anecdotal evidence from his own podcasting journey, including how listeners have approached him for demos after months of consuming his content, demonstrating the long-term, passive lead generation potential. The underlying methodology is that by consistently providing value and expertise through a podcast, one can cultivate an audience that trusts and respects them, making the eventual sales conversation much easier and more effective. Key Takeaways: * **Immediate Brand Recognition:** Podcasting offers a direct path to establishing personal or company brand recognition. By consistently producing content, individuals and organizations can become known to a target audience, fostering familiarity and recall. * **Create Your Own Platform:** Instead of seeking invitations to industry discussions, a podcast allows you to create your own "table," inviting experts and high-profile guests, thereby positioning yourself as a central figure in relevant conversations. * **Association with Expertise:** Hosting experts on your podcast allows you to associate your brand with their knowledge and credibility, enhancing your own perceived expertise even if you're not the sole subject matter expert on every topic. * **Represent Company Values:** Podcasting provides a unique medium to articulate and consistently demonstrate your company's core values, mission, and what you stand for, resonating with an audience that shares similar principles. * **Control the Conversation:** A podcast grants the host control over the topics discussed, the guests invited, and the overall flow of information, enabling strategic shaping of industry narratives and thought leadership. * **Value-Driven Selling:** Podcasting inherently focuses on providing free value, ideas, and insights rather than directly selling a product. This builds trust and positions the host as a helpful resource, making future sales conversations more natural and less transactional. * **Accelerated Rapport Building:** Regular listeners develop a sense of knowing, liking, and trusting the host over time, significantly shortening the rapport-building phase typically required in a traditional sales funnel. * **Instant Credibility:** Consistently hosting intelligent conversations and weighing in with valuable insights on a podcast establishes instant credibility, which is a powerful asset when engaging in sales discussions or attending industry events. * **Proactive and Passive Lead Generation:** Podcasting generates leads both directly (e.g., through calls to action or direct outreach to viewers) and passively (e.g., listeners reaching out after consuming content for an extended period), reducing the need for active prospecting. * **Perpetual Reusable Content:** A single podcast episode can be repurposed into multiple clips, articles, or social media posts, creating a vast library of evergreen content that can be used for lead nurturing, follow-ups, and ongoing marketing efforts in perpetuity. Key Concepts: * **Brand Recognition:** The extent to which a consumer can identify a brand by its name, logo, or other visual elements. Podcasting accelerates this by providing consistent exposure. * **Thought Leadership:** The position of being an authoritative expert in a particular field, whose expertise is sought out and whose opinions are respected. Podcasting facilitates this by allowing hosts to curate and lead discussions with other experts. * **Value-Driven Content:** Content that prioritizes providing free, useful, and insightful information to the audience, rather than directly promoting a product or service. This approach builds trust and long-term relationships. * **Sales Funnel Acceleration:** Strategies and tactics that shorten the time it takes for a prospect to move through the various stages of the sales process, from initial awareness to conversion. Podcasting achieves this through pre-built rapport and credibility. * **Content Repurposing:** The practice of taking existing content and transforming it into different formats or distributing it across various channels to maximize its reach and utility. A single podcast recording can yield numerous derivative content pieces. Examples/Case Studies: * **"Self-Funded" Podcast:** The speaker's personal podcast, which serves as a primary example of how he applies these principles to build his brand and generate leads. * **"Plan Site":** Mentioned as the speaker's company or product, indicating how his podcasting efforts directly support his business endeavors. * **"Stop-Loss Videos":** A previous content series created by the speaker, highlighting his history of creating valuable, niche-specific content to establish expertise.

IDMP in a capsule Tutorial
UNICOM
/@UNICOM-IDMP
Mar 24, 2022
This. The emphasis on patient safety and pharmacovigilance further underscores its relevance to medical affairs and regulatory compliance departments within their target market. This tutorial provides a comprehensive overview of the Identification of Medicinal Products (IDMP) standards, highlighting their crucial role in ensuring global medication safety. It explains how the ISO IDMP standards, though inconsistently implemented, are designed to work throughout a medicinal product's life cycle, from development and production to utilization and outcome assessment. Through illustrative stories, the video demonstrates how IDMP helps prevent adverse drug events, facilitates safe substitutions across different countries, curbs falsified medicines, and enhances global pharmacovigilance. A central theme is the concept of Medicinal Product Dictionaries (MPDs) as national repositories for comprehensive product information, linked globally by the Pharmaceutical Product Identifier (PHP ID), enabling seamless data navigation and personalized patient care through integration with personal health data. Key Takeaways: * **Standardized Global Identification is Critical:** Inconsistent identification of medicinal products across countries poses significant patient safety risks. IDMP provides a standardized framework (substance, dose form, strength, medicinal product, package) to ensure globally unique identification, crucial for safe healthcare and preventing errors. * **Medicinal Product Dictionaries (MPDs) as Central Data Hubs:** MPDs are vital national repositories that consolidate comprehensive product information (regulatory, scientific, pricing, dosage guidance). These dictionaries are the foundation for all information needed by hospitals, doctors, and pharmacies for safe prescribing and dispensing, and are accessed through various healthcare IT systems. * **The PHP ID Enables Cross-Border Data Linkage:** The Pharmaceutical Product Identifier (PHP ID) is a critical global identifier that allows for the seamless navigation and comparison of equivalent medicinal products across different national MPDs. This capability is essential for facilitating safe substitutions for patients traveling internationally and for aggregating global pharmacovigilance data. * **IDMP Supports Personalized Patient Safety:** By integrating IDMP-compliant product data from MPDs with individual patient health data (e.g., International Patient Summary - IPS), intelligent applications can provide real-time, personalized alerts for allergies, intolerances, and potential drug-drug interactions, significantly enhancing medication safety at the point of care. * **Enhanced Global Pharmacovigilance:** IDMP-compliant reporting, which includes the PHP ID and other identifiers, streamlines the aggregation and analysis of adverse drug event data globally. This enables faster identification of safety patterns, quicker responses (e.g., product recalls, updated warnings), and proactive risk mitigation across populations. * **Call for Industry-Wide Implementation:** The full benefits of IDMP, including improved medication safety and public health outcomes, can only be realized through widespread and consistent implementation by pharmaceutical companies, regulators, and IT solution providers across the entire medicinal product life cycle.

CTMS Oversight Deep Dive Demo
Veeva Systems Inc
/@VeevaSystems
Mar 22, 2022
This video provides a deep dive into Veeva Vault CTMS, showcasing its capabilities for comprehensive clinical trial oversight. It highlights how the platform facilitates effective collaboration, streamlines negotiations with CRO partners, and ensures regulatory compliance. The demonstration covers integrated study management, from initial planning and site activation to ongoing monitoring, risk assessment, and issue resolution. A central theme is the seamless integration between CTMS and TMF components, ensuring all clinical activities and documentation are managed within a unified, compliant system. The video also emphasizes robust data tracking, automated processes, and advanced reporting for real-time insights into study progress, site performance, and CRO oversight. Key Takeaways: * **Integrated Clinical Operations & Compliance:** Veeva Vault CTMS provides a unified platform for managing clinical trials, integrating CTMS and TMF functionalities to ensure seamless document management, regulatory compliance (e.g., 21 CFR Part 11 for signatures, automatic TMF artifact creation), and inspection readiness. * **Enhanced CRO and Vendor Oversight:** The system offers robust tools for managing and collaborating with CROs, including a global personnel directory for access control, automated notifications for CRO-submitted data (e.g., trip reports), dedicated issue logging against CROs, and dashboards for tracking vendor performance and issue resolution times.ai to offer AI-powered enhancements for predictive CRO performance, automated contract compliance checks, or intelligent issue triage. * **Proactive Risk Management & Issue Resolution:** The platform supports templatized risk assessments with automated scoring and integrated mitigation plans. It also provides comprehensive issue management capabilities, allowing for logging, assignment (including to CROs), tracking of resolution times, and trending analysis of quality findings and protocol deviations.ai could leverage AI/LLMs to enhance risk prediction, suggest optimal mitigation strategies, or automate the generation of issue summaries. * **Data-Driven Decision Making & Business Intelligence:** Extensive reporting and dashboard features provide real-time visibility into study progress, enrollment metrics, site performance, and TMF completeness. This enables data-driven decision-making, identification of at-risk milestones, and comparative analysis of CRO performance. * **Streamlined Workflow Automation:** The system automates several critical workflows, such as subject data calculation for actuals, automatic completion of milestones, generation of risk assessment documents, and creation of Part 11 compliant trip reports, significantly reducing manual effort and enhancing efficiency.

E3: xEVMPD Maintenance with Donika Doda
The Voice of Life Sciences
/@thevoiceoflifesciences1321
Mar 17, 2022
This video provides an in-depth exploration of xEVMPD (Extended Eudravigilance Medicinal Product Dictionary) maintenance, a critical regulatory compliance requirement for pharmaceutical companies operating within the European Union. Donika Doda, a Regulatory Affairs Specialist, discusses the complexities and strategies involved in making appropriate data submissions to the European Medicines Agency (EMA). The discussion highlights xEVMPD's role as the "mother of EMA databases," established in 2012 as part of Pharmacovigilance Legislation, serving as a central dictionary for medicinal product information and an interface for adverse event reporting. The conversation delves into the practicalities of xEVMPD maintenance, particularly how it fits into the post-approval phase of variation management. When a variation, such as a change to a Summary of Product Characteristics (SPC) or leaflet, is approved and impacts xEVMPD, companies are mandated to submit updated data to Eudravigilance within strict timelines (typically 15 or 30 days). Donika describes a largely manual process where Regulatory Affairs teams receive approved labeling, communicate the change, and then a designated person manually enters the database, finds the correct product, performs the update, and sends it to the EMA, awaiting an acknowledgment message. This manual process is underscored as a legal compliance obligation, crucial for ensuring healthcare professionals have access to the most current and accurate information, especially concerning safety variations. A significant portion of the discussion focuses on the challenges associated with xEVMPD maintenance. These include the inherent complexity of manual data entry, the need for precise timing, and the organizational hurdles arising from involving multiple departments like Pharmacovigilance and Regulatory Affairs. Donika emphasizes that the number of steps in the process directly impacts efficiency, advocating for streamlined workflows. A major pain point identified is the pervasive data duplication across various departmental software systems that often "do not talk to each other," leading to inefficiencies and wasted resources. This fragmentation necessitates a broader industry shift towards digital transformation. Looking to the future, the video introduces IDMP (Identification of Medicinal Products) as the "big brother" to xEVMPD, representing a significant opportunity for the industry to enhance efficiency and collaboration. IDMP is anticipated to facilitate a real interface between company software systems and the EMA, drastically reducing the time and effort required for data communication and maintenance. This upcoming standard is seen as a catalyst for companies to align their data, foster inter-departmental collaboration, and reduce duplication. The speakers advocate for companies to embrace this digital transformation, potentially by establishing dedicated teams responsible for managing this transition, ultimately leading to quicker access to reliable information for patients, healthcare professionals, and more efficient assessment processes for regulators. Key Takeaways: * **xEVMPD as a Core Regulatory Database:** The Extended Eudravigilance Medicinal Product Dictionary (xEVMPD) serves as the foundational "mother of EMA databases," centralizing medicinal product information and linking to pharmacovigilance for adverse event reporting. * **Mandatory Compliance for EU Operations:** Since 2012, xEVMPD maintenance has been a mandatory legal compliance requirement for all pharmaceutical companies with products registered in the European Union. * **Manual and Time-Sensitive Update Process:** Following the approval of variations (e.g., changes to SPC or leaflets), companies must manually update xEVMPD data within strict deadlines (15 or 30 days), involving regulatory affairs teams and direct communication with the EMA. * **Critical for Patient Safety and Healthcare Professionals:** Maintaining an up-to-date xEVMPD database is vital for patient safety, as healthcare professionals rely on this information from their respective authorities to ensure they have the latest details on prescribed or used products, especially for safety variations. * **Challenges of Inter-Departmental Complexity:** The maintenance process is complicated by involving multiple departments, such as Pharmacovigilance and Regulatory Affairs, highlighting the need for clear roles, responsibilities, and efficient communication channels. * **Inefficiencies Due to Data Duplication and Disparate Systems:** A significant challenge is the widespread duplication of information across different departmental software systems that lack interoperability, leading to wasted resources and increased effort. * **IDMP as a Catalyst for Digital Transformation:** The upcoming IDMP (Identification of Medicinal Products) standard is viewed as a major opportunity to drive digital transformation, promising a real interface between company software and the EMA, thereby reducing communication and maintenance times. * **Opportunity for Streamlined Operations and Collaboration:** IDMP implementation encourages companies to align data, foster greater collaboration between departments, and reduce data duplication, leading to more efficient internal operations. * **Need for Dedicated Digital Transformation Teams:** Companies are advised to consider establishing dedicated teams responsible for managing digital transformation initiatives to ensure a cohesive approach and successful adoption of new technologies and regulatory standards. * **Benefits of Digital Adoption:** Embracing digital transformation and implementing connectors between systems will reduce timing and effort, improve data reliability, and ultimately lead to quicker access to information for patients and healthcare professionals, as well as more efficient regulatory assessments. Key Concepts: * **xEVMPD (Extended Eudravigilance Medicinal Product Dictionary):** A mandatory EMA database containing information on all medicinal products registered in the European Union, serving as a central dictionary and linked to pharmacovigilance. * **Eudravigilance:** The European Medicines Agency's (EMA) system for managing and analyzing information on suspected adverse reactions to medicines authorized in the European Economic Area (EEA). * **EMA (European Medicines Agency):** The agency responsible for the scientific evaluation, supervision, and safety monitoring of medicines in the European Union. * **Pharmacovigilance:** The science and activities relating to the detection, assessment, understanding and prevention of adverse effects or any other medicine-related problem. * **IDMP (Identification of Medicinal Products):** A set of ISO standards for the unique identification of medicinal products, aimed at standardizing the way medicines are identified and described globally. * **SPC (Summary of Product Characteristics):** A document that describes the properties and the approved conditions of use of a medicinal product. * **Leaflet:** The patient information leaflet (PIL) that comes with a medicine, providing information on how to use it safely and effectively. * **Variation Management:** The process of managing changes to a medicinal product's marketing authorization after it has been approved. Tools/Resources Mentioned: * **Eudravigilance:** The database to which xEVMPD updates are submitted. * **Vault:** Mentioned as a potential platform where connectors might be built for future integration.
Behavior Modification in Healthcare
AHealthcareZ - Healthcare Finance Explained
@ahealthcarez
Mar 12, 2022
This video provides an in-depth exploration of behavior modification in healthcare, leveraging Professor BJ Fogg's renowned model. Dr. Eric Bricker, the presenter, begins by establishing the fundamental premise that improving health outcomes, quality, and reducing costs necessitates a change in human behavior. The core of the discussion revolves around applying Fogg's model—which posits that behavior change requires the simultaneous presence of Motivation, Ability, and a Trigger—to increase primary care utilization among members of employer-sponsored health plans. The presentation meticulously breaks down each component of the Fogg model, illustrating how a deficiency in any one area can prevent desired behavior change. Dr. Bricker uses a visual representation of Fogg's "action line," explaining that for difficult tasks, high motivation is required, while for easy tasks, low motivation suffices. Crucially, triggers only work when an individual is on the "right side" of this action line, meaning they possess sufficient motivation and ability. If a task is too hard or motivation is too low, triggers will fail, regardless of how frequently they are applied. Dr. Bricker then applies this framework to the real-world problem of low primary care engagement, citing statistics where only 15-50% of employees in large companies see a primary care physician within two years. He analyzes the current state, identifying that motivation is often low because the body is remarkably resilient, masking early signs of disease, and job-based incentives often fall flat due to general employee disengagement. Ability is severely hampered by the logistical difficulties of traditional primary care (time off work, travel, waiting, short doctor visits). Triggers are ineffective because they are typically generic and not personalized to individual needs, such as a 25-year-old male versus a 45-year-old female. The video concludes by outlining solutions for each component, drawing on the ancient Greek principles of persuasion (ethos, pathos, logos) for motivation, modern access solutions (on-site, virtual primary care) for ability, and personalized, multi-channel communication for triggers. The discussion culminates with a compelling case study of Serigraph, an automotive parts manufacturer that successfully kept its healthcare costs flat for nearly a decade by implementing these behavior modification strategies. Serigraph utilized a combination of monetary and time-off incentives, established an on-site clinic to drastically improve access and ease (ability), and employed "hyper-communication" through various channels, including mandated annual face-to-face coaching, to deliver highly personalized triggers. This real-world example underscores the practical applicability and profound impact of Fogg's model when systematically applied to healthcare challenges. Key Takeaways: * **BJ Fogg's Behavior Model (B=MAT):** Behavior change (B) is a product of Motivation (M), Ability (A), and a Trigger (T). All three elements must be present simultaneously for a behavior to occur. * **The "Action Line":** Fogg's model includes an "action line" on a graph where motivation (y-axis) and ability (x-axis) intersect. Behaviors above this line are more likely to occur with a trigger; those below will not, regardless of triggers. * **Motivation Challenges in Healthcare:** Individuals often lack motivation for preventative health due to the body's ability to mask disease symptoms until advanced stages. Generic job-based health incentives frequently fail to engage employees. * **Ability Barriers in Traditional Primary Care:** Accessing traditional primary care is often difficult, requiring significant time off work, travel, and waiting, making it a "half-day escapade" for a brief doctor interaction. This high effort severely limits ability. * **Ineffective Triggers:** Broad, non-personalized communication (e.g., mass emails) fails to resonate with diverse employee populations, as healthcare needs vary significantly by age, gender, and other demographics. * **Building Motivation through Persuasion:** Effective motivation for health comes from credible sources (doctors - Ethos), empathetic listening (Pathos), and then logical reasoning (Logos). Starting with logic without credibility and empathy is ineffective. * **Enhancing Ability with Accessible Care:** Making primary care "super easy" is crucial, especially for those with low motivation. Solutions include on-site clinics, near-site clinics, direct primary care, and virtual primary care, which reduce logistical barriers. * **Personalized Triggers are Essential:** Communication must be customized to the individual's needs and preferences. This can involve different channels (emails, texts, hard copies, spousal communication) and face-to-face coaching for tailored messaging. * **Triggers Fail Below the Action Line:** If motivation is low and ability is hard (below the action line), no amount of triggering (emails, texts, counseling) will result in behavior change; the foundational issues of motivation and ability must be addressed first. * **Serigraph Case Study - Integrated Approach:** The manufacturing company Serigraph successfully flattened healthcare costs for 10 years by combining incentives (monetary, time off), an on-site clinic (improving ability), and "hyper-communication" including mandated annual face-to-face coaching (personalized triggers). * **The Power of On-Site Clinics:** For concentrated workforces, on-site clinics significantly enhance ability by making care convenient, quick, and requiring no time off, which was a "crux" of Serigraph's success. * **Virtualization for Distributed Workforces:** For companies with geographically dispersed employees, virtual primary care is critical to replicate the "ease" factor of on-site clinics and overcome ability barriers. * **Conversations as Key to Customization:** Face-to-face coaching allows for highly customized triggers, as coaches can listen, empathize, and tailor their message based on individual conversations, addressing specific social determinants of health. * **Hyper-Communication Strategy:** Serigraph's success involved utilizing a multitude of communication channels—in-person meetings, emails, flyers, HR staff, managers—to ensure messages reached employees and their families effectively. Key Concepts: * **BJ Fogg's Behavior Model (B=MAT):** A framework stating that behavior change occurs when motivation, ability, and a trigger converge simultaneously. * **Action Line:** A graphical representation within Fogg's model indicating the threshold of motivation and ability required for a trigger to be effective. * **Ethos, Pathos, Logos:** Ancient Greek principles of persuasion: Ethos (credibility), Pathos (empathy), Logos (logic). The video emphasizes the importance of establishing ethos and pathos before presenting logos in healthcare communication. Examples/Case Studies: * **Serigraph:** An automotive parts manufacturer in Wisconsin that kept its healthcare costs flat for almost 10 years. Their strategy included monetary and time-off incentives, an on-site primary care clinic, and extensive, personalized communication including mandated annual face-to-face coaching.
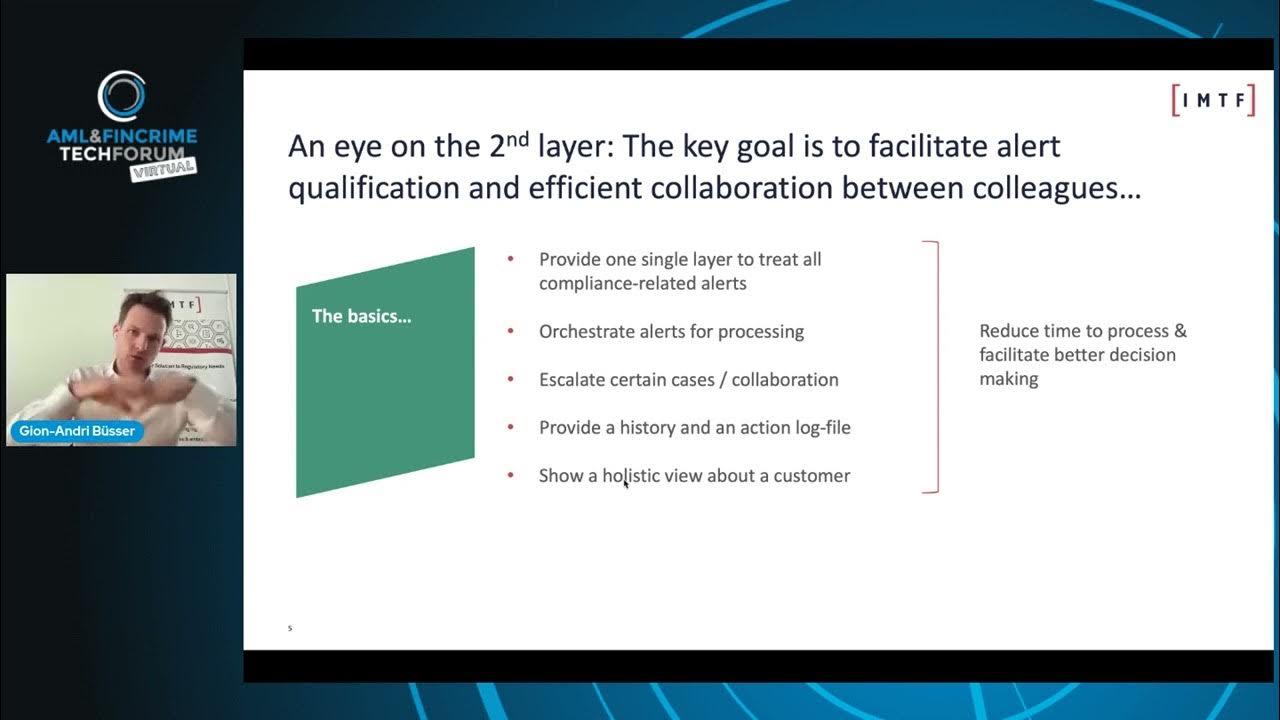
Benefits of a Two Layer Regulatory Intelligence Platform
IMTF - Excellence in RegTech Solutions
/@imtf-excellenceinregtech
Mar 11, 2022
The speaker, Gion-Andri Büsser of IMTF, discusses the critical need for modern technology in compliance, driven by exploding costs of compliance and even higher costs of non-compliance. He introduces a "two-layer regulatory intelligence platform" concept, emphasizing an orchestration layer that centralizes the treatment of compliance alerts, automates processes, fosters collaboration, and provides a holistic view of data. The video highlights how advanced technologies, including machine learning and data science, can be leveraged within this architecture to significantly reduce manual work, improve efficiency, and enhance risk management. Key Takeaways: * **Ecosystem Approach to Compliance Technology:** The video advocates for viewing compliance technology as an integrated ecosystem rather than disparate, siloed software packages. This platform approach is crucial for comprehensive data utilization and decision-making. * **The Power of the Orchestration Layer (Layer 2):** A dedicated orchestration layer is presented as essential for consolidating and processing all compliance alerts (e.g., AML, fraud, sanctions), enabling flexible process automation, fostering collaboration across teams, and maintaining accurate, regulator-ready audit trails. * **AI/ML for Enhanced Efficiency and Risk Reduction:** The "magic" of the orchestration layer lies in its ability to leverage AI and machine learning for advanced functions such as intelligent auto-closure of routine alerts, pre-processing to highlight historical patterns, and more granular, accurate risk rating based on comprehensive customer history. * **Strategic IT and Change Management Benefits:** Implementing an orchestration layer provides significant IT flexibility, allowing organizations to introduce modern tools and interfaces without immediately replacing existing, potentially valuable, legacy detection systems (Layer 1). This enables a phased modernization approach, reducing disruption and risk. * **Continuous Adaptation to Evolving Threats:** The speaker underscores that financial crime and compliance challenges are an "ever-ending battle," with criminal behaviors constantly evolving (e.g., due to pandemics, crypto). This necessitates adaptive, forward-looking technology to anticipate and combat new threats.g., GxP, 21 CFR Part 11, FDA/EMA regulations).

Veeva Systems (VEEV) Stock Analysis and Intrinsic Value | Buy Now or Wait?
Andrew Finance
/@andrewfinance5351
Mar 11, 2022
This video provides a detailed financial and technical analysis of Veeva Systems (VEEV) stock, assessing its intrinsic value using Discounted Cash Flow (DCF) and Earnings Per Share (EPS) models under various performance scenarios. It delves into Veeva's business strengths, risks, and future growth prospects, ultimately providing an investment recommendation. The analysis highlights Veeva's strong market position as a cloud-computing leader in the pharmaceutical and life sciences industries, its robust financial health, and its strategic expansion into other regulated sectors. Key Takeaways: * **Veeva's Dominance in Life Sciences:** Veeva Systems is firmly established as a leading cloud-computing provider for the pharmaceutical and life sciences industries, characterized by strong subscription revenue, high switching costs, and a strategic relationship with Salesforce, which limits competition in its core niche. * **Robust Financial Health and Growth Outlook:** The company demonstrates excellent profitability with a 23% profit margin, 11% return on assets, and 15% return on equity, coupled with a strong balance sheet. It is projected to achieve significant revenue growth (14% yearly) and EPS growth (10% yearly) over the next five years, indicating a healthy and expanding ecosystem for Veeva-centric solutions. * **Strategic Market Expansion:** Veeva has begun extending its content and data management solutions beyond life sciences into other regulated sectors such as consumer goods, chemicals, and cosmetics, signaling potential future growth avenues and broader applicability of its platform. * **Competitive Landscape and Operational Risks:** Despite its specialized market, Veeva faces competition from major enterprise software vendors like Oracle and Microsoft. Key risks include potential slowdowns in near-term growth due to labor pressures or challenges in closing large deals, customer churn, commercial execution issues, and litigation. * **Market Valuation Perspective:** The analysis concludes that Veeva stock is currently overvalued, recommending investors wait for signs of reversal or a price drop below $130 before considering an investment.

Almost HALF of Cardiovascular Disease in Diabetes NOT TREATED!!
AHealthcareZ - Healthcare Finance Explained
@ahealthcarez
Mar 5, 2022
This video provides an in-depth exploration of the alarming under-treatment of cardiovascular disease (CVD) in patients with diabetes, despite the availability of highly effective and affordable medications. Dr. Eric Bricker begins by outlining the pathophysiology of atherosclerosis, explaining how diabetes exacerbates the hardening and narrowing of arteries, leading to critical conditions such as heart attacks, strokes, and peripheral vascular disease (PVD). He emphasizes that PVD, often affecting the feet, can result in non-healing ulcers, gangrene, and amputations, while strokes are essentially "heart attacks of the brain" caused by similar atherosclerotic processes. The speaker highlights that this disease is "silent," meaning patients often feel fine until a catastrophic event occurs, making proactive treatment crucial. The presentation then details three categories of evidence-based treatments for diabetic patients with atherosclerosis: statin medications (e.g., Lipitor, Crestor) for cholesterol lowering, ACE inhibitors or Angiotensin Receptor Blockers (ARBs) for blood pressure control and organ protection (heart, blood vessels, kidneys), and newer medications like SGLT2 inhibitors and GLP-1 receptor antagonists that improve outcomes. The core issue is revealed through a study published in the Journal of the American Medical Association (JAMA) in February 2022. This study, encompassing hundreds of thousands of patients across 12 hospital systems, found that a staggering 43% of individuals with diabetes and cardiovascular disease received *zero* evidence-based treatments. Furthermore, only 20% received both statins and ACE inhibitors/ARBs, despite these being generic, "dirt cheap," and available for decades. Dr. Bricker critically examines the reasons behind this significant "gap in evidence-based care." He argues that the problem is not a lack of medical discovery but a profound failure in implementation within the American healthcare system. He points out that the fee-for-service payment model offers no accountability for doctors to follow evidence-based guidelines. Even existing value-based payment programs, including commercial and Medicare initiatives, are failing to move the needle on these statistics. Given that diabetes prevalence is growing (from 8% to 13% of adults in America over 20 years), this under-treatment represents a massive and escalating problem. The speaker concludes by asserting that employers, who bear the financial risk for their employees' health plans, must "own this problem" of implementation, as it is solvable and directly impacts their financial burden and employee well-being. Key Takeaways: * **Widespread Under-treatment:** A JAMA study revealed that 43% of patients with diabetes and cardiovascular disease receive no evidence-based treatments, and only 20% receive the two well-established, affordable treatments (statins and ACE inhibitors/ARBs). * **Pathophysiology of Atherosclerosis:** Diabetes significantly worsens atherosclerosis (hardening and narrowing of arteries) by making cholesterol plaques "extra sticky," while hypertension increases the likelihood of these plaques rupturing, leading to severe blockages. * **Consequences of Untreated Atherosclerosis:** This silent disease can lead to heart attacks, strokes, peripheral vascular disease (causing non-healing foot wounds, gangrene, and amputations), and kidney failure requiring dialysis. * **Effective and Affordable Treatments Exist:** Established treatments like statins (cholesterol-lowering) and ACE inhibitors/ARBs (blood pressure and organ protection) have been available for over two decades, are generic, and are "dirt cheap," often costing just a few dollars a month. Newer medications like SGLT2 inhibitors and GLP-1 receptor antagonists also improve outcomes. * **"Gaps in Evidence-Based Care":** This medical jargon refers to the failure to implement known, effective treatments that prevent severe cardiovascular events and complications in diabetic patients. * **Implementation Problem, Not Discovery Problem:** The core issue is not a lack of scientific discovery or effective medications, but rather a systemic failure in the healthcare infrastructure to ensure these proven treatments are consistently applied to patients who need them. * **Failure of Current Payment Systems:** The fee-for-service model provides no accountability for physicians to adhere to evidence-based guidelines. Critically, even existing value-based payment programs in commercial insurance and Medicare are not effectively addressing these treatment gaps. * **Growing Public Health Crisis:** The prevalence of diabetes in American adults has increased significantly (from 8% to 13% in 20 years), exacerbating the impact of this under-treatment problem on individuals and the healthcare system. * **Employers Bear Financial Risk:** Employers sponsoring health plans are ultimately responsible for the financial burden of poor patient care and preventable complications arising from untreated cardiovascular disease in their diabetic employees. * **Call to Action for Employers:** Employers are urged to "own this problem" of implementation, as it is solvable and crucial for reducing their financial risk and improving the health of their plan members. * **Physician Engagement is Key:** The study found that 75% of these under-treated patients had been seen by a primary care physician or cardiologist, indicating that the issue often lies with physician adherence to guidelines or patient engagement strategies. Tools/Resources Mentioned: * Journal of the American Medical Association (JAMA) - cited study from February 17, 2022. * CDC National Diabetes Statistics Report - referenced for diabetes prevalence data. Key Concepts: * **Atherosclerosis:** A disease in which plaque builds up inside your arteries, causing them to harden and narrow, restricting blood flow. * **Peripheral Vascular Disease (PVD):** A circulatory condition in which narrowed blood vessels reduce blood flow to the limbs, often leading to non-healing wounds, ulcers, and potential amputation. * **Statins:** A class of drugs used to lower cholesterol levels in the blood. * **ACE Inhibitors (Angiotensin-Converting Enzyme Inhibitors) / ARBs (Angiotensin Receptor Blockers):** Medications primarily used to treat high blood pressure and heart failure, also protective for the heart, blood vessels, and kidneys. * **SGLT2 Inhibitors / GLP-1 Receptor Antagonists:** Newer classes of medications for diabetes that have also shown significant cardiovascular and renal benefits. * **Evidence-Based Care:** Medical care that is supported by clinical research and scientific evidence. * **Fee-for-Service:** A payment model where healthcare providers are paid for each service they provide. * **Value-Based Payment:** A payment model that rewards healthcare providers for quality of care and patient outcomes, rather than quantity of services.
TMF & Quality Control
Power of Work
/@powerofwork6914
Mar 4, 2022
This video provides a comprehensive overview of Trial Master File (TMF) quality control (QC) within clinical trials, emphasizing its critical role in regulatory compliance and drug approval. The speaker details how TMF documentation serves as proof of a drug's safety and efficacy, ensuring adherence to Good Clinical Practices (GCP) and ICH guidelines. The discussion covers the practical aspects of TMF management, including the use of electronic TMF (eTMF) systems like Veeva, the importance of TMF maps and plans for document organization, and the meticulous process of performing QC checks. These checks involve verifying document completeness, correct filing, metadata accuracy, and the presence of required signatures, all while safeguarding patient privacy. The video highlights the challenges of managing vast amounts of documentation and the necessity for rapid document retrieval during audits and inspections. Key Takeaways: * **TMF as a Regulatory Cornerstone:** The TMF is indispensable for demonstrating regulatory compliance (FDA, ICH, GCP) in clinical trials, serving as the primary evidence for drug safety, efficacy, and patient protection. * **Operational Efficiency through Organization:** Effective TMF management, utilizing tools like the TMF Reference Model and company-specific TMF plans, is crucial for maintaining organized documentation and enabling rapid retrieval, which is vital during audits and inspections. * **Meticulous Quality Control is Paramount:** A rigorous QC process for TMF documents is essential, focusing on completeness, accurate metadata, correct filing, signature verification, and the absence of Protected Health Information (PHI) to ensure audit-readiness. * **Veeva's Role in eTMF Management:** The video explicitly mentions Veeva as a common system for managing eTMFs, underscoring the prevalence of specialized software in handling the complexities of clinical trial documentation. * **Challenges and Opportunities for Automation:** The manual and time-intensive nature of TMF QC, coupled with the high volume and complexity of documents, presents significant challenges that could be addressed through advanced automation and AI solutions for classification, metadata extraction, and compliance checks. * **The "Gatekeeper" Role of TMF Processors:** Document specialists act as critical "gatekeepers," ensuring the integrity and accuracy of the TMF, identifying discrepancies, and clearly documenting findings for resolution by document owners, thereby upholding the overall quality of clinical trial records.

Investing in Companies that Earn Profits #veeva #iqvia #nvidia #thermofisher #adobe
Animal Donut
/@animaldonut
Feb 24, 2022
This video provides an in-depth exploration of how to identify profitable companies for long-term investment, moving beyond mere stock price fluctuations to focus on underlying business fundamentals. The speaker, Jeff Luke, a professional photographer and author of "Stock Market Intelligence," aims to equip investors with tools to analyze a company's financial health. He emphasizes the importance of understanding revenues, operating expenses, and net income to determine true profitability, contrasting this approach with speculative investing in companies that may not yet be generating profits. The core message is that long-term investment success is rooted in becoming a part-owner of a fundamentally sound, profitable business. The presentation progresses by first setting the stage for a more informed investment strategy, highlighting the distinction between short-term market "voting" (price movements) and long-term "weighing" (business fundamentals). Luke then illustrates his methodology by examining five specific companies, all of which he personally holds stock in, providing their trailing 12-month (TTM) revenues, operating income, and net income. He explicitly mentions his preference for investing in industries he understands well, particularly the life sciences, which informs his selection of companies like Veeva Systems, Iqvia, and Thermo Fisher Scientific. This approach underscores the value of industry knowledge in making confident, long-term investment decisions. The video details the financial performance and market positioning of each selected company. Veeva Systems is highlighted as a leading provider of cloud-based software for the life sciences industry, known for its profitability. Iqvia is presented as a dominant contract research organization (CRO) and a key player in life sciences data and analytics. Nvidia's role as a top designer of GPUs, crucial for enhancing visual computing and powering technologies like autonomous vehicles, is discussed. Thermo Fisher Scientific is identified as the premier life sciences supplier, offering a vast portfolio of devices and machinery for scientific analysis. Finally, Adobe Systems is recognized for its dominance in content creation software through its Creative Cloud subscription model. For each, specific financial figures are provided, reinforcing the video's focus on tangible profitability metrics. Ultimately, the video advocates for a disciplined, fundamental-driven investment strategy. Luke encourages viewers to always ascertain a company's profitability before investing, fostering a category of investor who makes decisions based on clear financial understanding rather than chasing "hot stocks." He stresses that investing in well-run, profitable businesses provides confidence, reduces the need for constant market monitoring, and aligns with a long-term holding strategy, allowing investors to "buy it and then just put it away." Key Takeaways: * **Prioritize Profitability in Investing:** Investors should always determine if a company is earning profits or suffering losses before making an investment, moving beyond mere stock price movements to understand the underlying business health. * **Understand Core Financial Metrics:** Key indicators of a company's financial health include revenues (money taken in), operating income (money left after operating expenses), and net income (final profit after all costs). These are crucial for assessing true profitability. * **Access Financial Data:** Basic financial statement information, including income statements, can be found on a company's website (annual/quarterly reports) or through financial services like Value Line and Morningstar. * **Veeva Systems' Market Position:** Veeva is a profitable, leading provider of cloud-based software solutions specifically for the life sciences industry, making it a significant player in a specialized and regulated sector. * **Iqvia's Dominance in Life Sciences:** Iqvia is a profitable and dominant contract research organization (CRO) and a key player in life sciences data and analytics, serving a critical role in drug development and healthcare insights. * **Nvidia's GPU Leadership:** Nvidia is the top designer of Graphics Processing Units (GPUs), which are essential for enhancing visual computing platforms and are increasingly vital for AI applications, including autonomous vehicles. * **Thermo Fisher Scientific as a Life Sciences Giant:** Thermo Fisher Scientific is described as the premier life sciences supplier, providing a wide array of devices, machinery, and services used for analysis and research within the life sciences industry. * **Adobe's Content Creation Monopoly:** Adobe Systems dominates the content creation software market with iconic products like Photoshop and Illustrator, operating on a successful subscription model (Creative Cloud). * **Speaker's Investment Philosophy:** The speaker, Jeff Luke, emphasizes investing in industries one understands well (e.g., life sciences) to better grasp a company's relative strength and dominance, leading to more confident, long-term investment decisions. * **Long-Term vs. Short-Term Investing:** The video distinguishes between short-term market "voting" (speculation based on price) and long-term "weighing" (investment based on business fundamentals and profitability), advocating for the latter. * **Confidence in Well-Run Companies:** Investing in consistently profitable and well-run companies provides confidence, reducing the need for frequent trading decisions and allowing for a "buy it and put it away" long-term strategy. * **Avoid Speculation Without Awareness:** While speculating on unprofitable companies is an option, investors should be fully aware of the inherent risks and understand that such ventures are not based on current profitability. Tools/Resources Mentioned: * Company annual reports * Company quarterly reports * Value Line (financial research service) * Morningstar (financial research service) * "Stock Market Intelligence" (book by Jeff Luke) * "Crush It With ETFs" (book by Jeff Luke) * "The ETF Investor" (book by Jeff Luke) * Sony ZV-1 (camera used for filming) * Joby TelePod Mobile Tripod (tripod used for filming) Key Concepts: * **Revenues:** The total amount of money a company generates from its sales of goods or services before any expenses are deducted. * **Operating Income:** A company's profit after subtracting operating expenses (such as wages, depreciation, and cost of goods sold) from revenues, but before deducting interest and taxes. * **Net Income:** The total profit of a company after all expenses, including operating costs, interest, and taxes, have been deducted from revenues. Often referred to as "the bottom line." * **Trailing 12 Months (TTM):** A financial metric that represents the sum of a company's financial performance over the past 12 consecutive months, providing a more current view than annual reports. * **Contract Research Organization (CRO):** An organization that provides support to the pharmaceutical, biotechnology, and medical device industries in the form of research services outsourced on a contract basis. * **Graphics Processing Unit (GPU):** A specialized electronic circuit designed to rapidly manipulate and alter memory to accelerate the creation of images in a frame buffer intended for output to a display device. GPUs are crucial for AI and machine learning. * **Creative Cloud:** Adobe's subscription service that provides users with access to a collection of software developed by Adobe for graphic design, video editing, web development, photography, and more. * **"Voting" vs. "Weighing":** An investment analogy where "voting" refers to the short-term market sentiment and price fluctuations (how the market "votes" on a stock), while "weighing" refers to the long-term assessment of a company's intrinsic value based on its fundamentals (how the market "weighs" the business over time).

Leveraging Your Veeva Vault Investment
Daelight Solutions
/@daelightsolutions2128
Jan 24, 2022
This video provides an in-depth exploration of maximizing investment in Veeva Vault, a critical platform for life sciences companies. Presented by Daelight Solutions, an IT consulting company specializing in life sciences, the webinar focuses on the technical and business considerations required when adding new functional capabilities, applications, or integrating systems within an existing Veeva Vault environment. The speakers, Dan Wheeler (Founder and CEO) and Terry Montez (Clinical Practice Lead), share their expertise and real-world insights, emphasizing that the "go-live" of a Veeva Vault implementation is merely the beginning of an ongoing journey that requires strategic planning and disciplined management. The presentation begins by outlining the typical customer journey with Veeva Vault, from initial planning and design through configuration, build, testing, and eventual go-live. It then transitions to highlight the continuous nature of managing a Veeva Vault investment, which includes navigating three annual releases, user-specific enhancements, shifts in business direction (e.g., acquisitions, insourcing TMF), future integrations, and the expansion into additional Veeva Vault suites or applications. To manage this inherent complexity, the speakers introduce a robust framework centered on roadmaps, change management, and solution governance, stressing that proactive planning is paramount to avoid chaos and ensure long-term success. The core of the webinar delves into practical examples and case studies from Daelight Solutions' client engagements. These examples illustrate common challenges and best practices when expanding Veeva Vault usage, such as adding Study Startup (SSU) or Clinical Trial Management System (CTMS) to an existing eTMF Vault, integrating Registrations into a Submissions Vault, deploying new Vault suites (Clinical, Quality, Regulatory) simultaneously, and leveraging advanced features like SiteConnect. Each case study provides specific details on issues encountered—like data model inconsistencies, legacy data migration complexities, global directory duplications, and the need for cross-functional alignment—along with actionable recommendations for overcoming them, underscoring the critical role of data governance and early stakeholder collaboration. Key Takeaways: * **Go-Live is Just the Beginning:** A Veeva Vault implementation's go-live marks the start of a continuous journey involving annual releases, user enhancements, business shifts (e.g., acquisitions, insourcing TMF), and potential future integrations or expansions into additional Vault suites and applications. * **Robust Roadmaps are Essential:** Develop a comprehensive roadmap aligned with company strategies and objectives, securing buy-in from executive sponsors and cross-functional leads. This roadmap must include realistic timelines, budgets, and a strong focus on change management, training, and communication to ensure widespread adoption. * **Disciplined Change Management:** Implement a formal release management plan that clearly defines roles and responsibilities for IT, business, validation, and quality partners. Utilize a Change Advisory Board (CAB) to prioritize changes, assess the impact of Veeva releases, and strategically defer requests if out-of-the-box functionality is imminent, aiming to keep solutions as standard as possible. * **Strong Solution and Data Governance:** Establish robust solution governance to ensure compliance with industry regulations (FDA, EMA, GxP, 21 CFR Part 11) and best practices. Crucially, implement data governance (people, process, technology) to define naming conventions, manage master data (e.g., organizations, personnel), and maintain consistency across all Vaults, especially for shared data. * **Early Planning Prevents Rework:** When adding new applications (e.g., SSU to eTMF), engage all stakeholders and conduct thorough analysis *before* configuration. This includes re-evaluating TMF index, milestone sets, and EDLs to build a foundational structure that accommodates future functionality and avoids costly rework. * **Thorough Data Model Analysis for Integrations:** For applications with distinct data models (e.g., product-based Registrations versus submission-based Submissions), perform in-depth data model analysis upfront. Understand how new data structures will expand and impact existing models, and address legacy data integrity issues at the source prior to migration. * **Engage Experts for Complex Processes:** When business processes or data usage are unclear, particularly for complex systems like Registrations, engage experts (e.g., from Veeva) to understand downstream data utilization. This insight helps inform configuration decisions and ensures the system meets long-term business needs. * **Test with Diverse Scenarios:** Before full rollout, manually test new configurations by adding a few diverse product types or scenarios. This iterative testing helps work out kinks, validate data organization, and ensures the system functions as expected across various use cases. * **Cross-Suite Standard Alignment:** When deploying multiple Vault suites (e.g., Clinical, Quality, Regulatory), dedicate significant effort to aligning on support processes, data sharing standards, SOP updates, and standard terminology across all domains from the outset. Early and continuous participation from all affected groups is critical. * **Centralize Vault Management:** To minimize confusion and service impact, centralize the management of all Veeva Vaults, including terminology, naming conventions, object relationships, and communication standards. This provides a consistent framework for IT support and users, even if initial naming choices were suboptimal. * **Strategic SiteConnect Implementation:** For SiteConnect, define clear business decisions regarding document flow (site to sponsor, sponsor to site), internal connectivity for regulatory/safety documents, and document packages to be shared. Adapt internal processes (e.g., site connection states) and SOPs to accommodate a hybrid environment of sites using and not using SiteVault. * **Anticipate Global Directory and User Provisioning Impacts:** Integrating external systems like SiteConnect significantly impacts global directory structures (e.g., shifting from hospital names to department-specific organizations, incorporating USN numbers) and user provisioning processes, requiring data reformatting and new rules. * **Leverage Cloud Platform for Third-Party Exchange:** For exchanging data with third parties not using specific Veeva connectors, consider leveraging underlying cloud platform capabilities (e.g., AWS Lambda and S3 storage) to automate data ingestion, transform data into Vault-loader-ready formats, and streamline the transfer process. * **Consider Veeva Platform Vault for Non-GxP Documents:** For managing documents that don't fit neatly into existing development cloud vaults (e.g., legal contracts, budgets), explore Veeva's platform vault offering. This can provide a single platform and consistent user experience for both GxP and non-GxP content, but should be discussed with Veeva account managers. **Tools/Resources Mentioned:** * Veeva Vault (general platform) * Veeva CRM * Veeva Clinical (eTMF, CTMS, SSU, SiteConnect, MyVeeva Patient application) * Veeva Regulatory (Submissions, Registrations) * Veeva Quality (QualityDocs, QMS) * Veeva PromoMats * Amazon Web Services (AWS) functionality: Lambda, S3 storage * Vault Loader **Key Concepts:** * **Veeva Vault:** A cloud-based content and data management platform specifically designed for the life sciences industry, offering various suites and applications. * **eTMF (electronic Trial Master File):** A digital system for managing essential clinical trial documents, ensuring compliance and audit readiness. * **SSU (Study Startup):** The phase of clinical trials involving all activities required to initiate a study, including site selection, contract negotiation, and regulatory approvals. * **CTMS (Clinical Trial Management System):** Software used to manage and track various aspects of clinical trials, including participant enrollment, site performance, and study progress. * **Registrations:** The process of tracking and managing product registrations with regulatory authorities worldwide. * **Submissions:** The process of preparing and submitting regulatory documents (e.g., eCTD) to health authorities. * **SiteConnect:** A Veeva solution that facilitates the secure exchange of documents and data between sponsor Veeva Vaults and investigator SiteVaults. * **Global Directory:** A centralized repository within Veeva Vault for managing information about organizations, sites, and personnel, crucial for consistent data across applications. * **Country Intelligence:** A feature within Veeva Vault that provides guidance and control for managing country-specific regulatory requirements and document collections. * **Master Data Management (MDM):** A comprehensive method for defining and managing an organization's critical non-transactional data to provide a single point of reference. * **Change Advisory Board (CAB):** A formal group responsible for reviewing, evaluating, authorizing, and prioritizing changes to IT services and infrastructure, including Veeva Vault configurations and releases. * **GxP, 21 CFR Part 11, FDA, EMA:** Regulatory standards and authorities relevant to pharmaceutical and life sciences industries, emphasizing good practices (GxP), electronic records and signatures (21 CFR Part 11), and oversight by the Food and Drug Administration (FDA) and European Medicines Agency (EMA).

Veeva Systems: Case Study in Converting to a Public Benefit Corporation
UC Berkeley School of Law
/@UCBerkeleySchoolofLaw
Jan 20, 2022
This video provides an in-depth exploration of Veeva Systems' groundbreaking conversion to a Public Benefit Corporation (PBC) in January 2021, making it the first public company to do so with 99% shareholder support. The content serves as an accompaniment to a Berkeley Law Executive Education case study, delving behind the scenes of this significant corporate governance shift. The discussion features insights from Veeva's founder, who shares personal anecdotes and the philosophical underpinnings of the decision, alongside expert commentary on the legal and economic implications of the PBC structure. The core of the video centers on the evolution of corporate responsibility from traditional shareholder primacy to a more expansive stakeholder-centric model. Veeva's founder recounts his early experiences in a small family business, where taking care of customers and the community was paramount due to the lack of an external safety net, contrasting this with the overly simplistic "make money for shareholders and don't do anything illegal" mandate of traditional corporate charters. The concept of a PBC is introduced as an innovative legal framework that allows a company's board to explicitly balance the interests of various stakeholders—including employees, customers, the community, and the environment—with those of shareholders, even when trade-offs are involved. The video emphasizes that formalizing a company's social purpose and values in its articles of incorporation, as a PBC does, serves multiple critical functions. It provides a clearer communication mechanism for a growing workforce and customer base, sets a legal obligation for future leadership, and ensures the company's ethos remains consistent over decades. The conversion process at Veeva involved extensive internal discussions, including a pivotal hike with the chairman of the board, and careful communication with investors. Surprisingly, investors were not skeptical once the rationale was thoroughly explained, recognizing the long-term benefits of a company that is clear about its social purpose and committed to ethical governance. The benefits of this shift, as articulated in the video, extend beyond mere ethical considerations to tangible business advantages. Companies with a clear social purpose are better equipped to manage stakeholder expectations, align business strategy with corporate purpose, secure a durable social license to operate, communicate more authentically, and proactively flag risks. For Veeva, the PBC status has already yielded positives such as attracting employees aligned with its values, deepening customer relationships, and significantly increasing the source of innovative ideas by prompting consideration of value-aligned initiatives alongside business growth. The video concludes by highlighting that while a PBC is a powerful mechanism, the fundamental principle is clear social purpose, accountability, and reporting, which can also be pursued within traditional corporate forms, especially as shareholders increasingly advocate for stakeholder focus. Key Takeaways: * **Pioneering Corporate Governance:** Veeva Systems became the first public company to convert to a Public Benefit Corporation (PBC) in January 2021, with overwhelming support (99%) from its voting shareholders, setting a precedent for publicly traded entities. * **Redefining Corporate Purpose:** A PBC legally mandates that a company's board of directors can balance the interests of all stakeholders (employees, customers, community, environment) with those of shareholders, moving beyond the sole focus on shareholder primacy inherent in traditional corporate structures. * **Formalizing Values for Longevity:** Converting to a PBC allows a company to formalize its values and social purpose within its articles of incorporation, ensuring that these principles are legally binding and communicated clearly to employees, customers, and future leadership, fostering long-term consistency. * **Strategic Communication and Risk Management:** Companies with a clear social purpose, like PBCs, are better positioned to manage stakeholder expectations, align business strategies, build a strong social license to operate, communicate authentically, and effectively identify and mitigate risks. * **Shareholder Alignment with Stakeholder Focus:** Counter-intuitively, many investors are not skeptical of the PBC model; when properly explained, they recognize that a strong commitment to social purpose and stakeholder well-being can lead to long-term economic sustainability and reduced risk. * **Enhanced Attractiveness for Talent and Customers:** Veeva experienced tangible benefits, including attracting employees who are aligned with the company's values and deepening relationships with customers, which are crucial for sustained growth and market leadership. * **Innovation Through Values:** The PBC framework has broadened Veeva's source of ideas, encouraging the pursuit of initiatives aligned with its values, which are then cross-referenced with business objectives, fostering a more holistic approach to innovation. * **Complexity of Balancing Interests:** While beneficial, balancing the diverse interests of multiple stakeholders presents new and unprecedented challenges for management and boards compared to the simpler focus on shareholder primacy, requiring more information gathering and trust-building. * **Internal Ethos is Crucial:** For a PBC to be effective, its charter must genuinely align with the company's internal ethos and way of working; imposing a charter externally without internal buy-in can lead to operational issues. * **Formalized Stakeholder Communication:** The PBC structure formalizes communication channels with stakeholders, breaking down corporate silos and providing boards with a wider array of viewpoints and information essential for making informed decisions. * **Accountable Reporting:** PBCs are required to report on their pursuit of their public benefit purpose, emphasizing accountability over mere positive optics, with the understanding that this will be an iterative process requiring shareholder feedback. * **Broader Definition of Social Purpose:** The video expands the definition of "social purpose" beyond merely avoiding negative externalities (like pollution or discrimination) to include a company's broader obligations to society, such as protecting democracy. * **Economic Sense for Diversified Shareholders:** From the perspective of a diversified shareholder, investing in companies that manage stakeholders well and do not externalize costs makes economic sense, as such externalizations can negatively impact other companies within their portfolio. Key Concepts: * **Public Benefit Corporation (PBC):** A legal corporate structure that requires a company to balance the financial interests of its shareholders with the best interests of its stakeholders (employees, customers, community, environment) and a specific public benefit purpose. * **Shareholder Primacy:** The traditional corporate governance theory that a company's primary responsibility is to maximize profits for its shareholders. * **Stakeholder Capitalism:** An economic system in which companies are oriented to serve the interests of all their stakeholders, not just shareholders. * **Social Purpose:** The idea that companies should serve a purpose beyond profit generation, contributing positively to society and the environment. * **Corporate Governance:** The system of rules, practices, and processes by which a firm is directed and controlled, encompassing the relationship between management, its board of directors, shareholders, and other stakeholders. * **Externalities:** Costs or benefits incurred by a third party who is not directly involved in a transaction or activity (e.g., pollution affecting local communities). Examples/Case Studies: * **Veeva Systems' PBC Conversion:** The entire video serves as a case study of Veeva Systems' journey to becoming the first public company to convert to a Public Benefit Corporation, detailing the motivations, process, and initial outcomes.

Smart Classifier: Bulk Classification & Data Segregation
NextLabs
/@NextLabsInc
Jan 13, 2022
This video introduces NextLabs’ Smart Classifier, a tool designed for bulk classification, organization, and protection of documents in shared folders and SharePoint sites. It emphasizes the importance of a strong data governance framework for data safety and productivity, showcasing how the Smart Classifier streamlines data management processes. The system operates through file watchers, content extractors, and rule engines to automatically classify files based on their content or metadata. The demonstration highlights two key use cases: bulk classification of existing documents (e.g., ITAR/EAR) to enforce attribute-based access control (ABAC) policies, and automated data segregation, where classified documents are moved to designated "system of record" folders. The solution ensures sensitive data is secured with fine-grained access controls and digital rights protection, preventing unauthorized disclosure. * **Scalable Compliance and Security:** The ability to classify and protect documents in bulk, using rules based on content or metadata, addresses the challenge of managing vast volumes of sensitive data. This scalability is essential for pharmaceutical companies dealing with large datasets from R&D, clinical trials, and commercial operations, ensuring consistent application of security and compliance policies. * **Enhanced Data Quality and Management:** By automating classification and segregation, the solution improves data quality and streamlines data management processes. * **Fine-Grained Access Control (ABAC) for Sensitive Data:** The integration of attribute-based access control (ABAC) allows for dynamic, fine-grained control over sensitive documents, preventing unauthorized disclosure. This is crucial for protecting intellectual property, patient data, and other confidential information within the life sciences sector * **Addressing Legacy Data Challenges:** The video highlights the challenge of classifying existing, unclassified files. Smart Classifier's bulk classification feature provides a solution for bringing legacy data into compliance, a common pain point for established pharmaceutical companies.
![[Webinar] Automating Clinical Trial Master File Migration & Information Extraction](https://i.ytimg.com/vi/IchcgkDDdtw/hqdefault.jpg?sqp=-oaymwEcCNACELwBSFXyq4qpAw4IARUAAIhCGAFwAcABBg==&rs=AOn4CLD8QvOyM_6WqAniWDO0HGPWtHJEqw)
[Webinar] Automating Clinical Trial Master File Migration & Information Extraction
John Snow Labs – Healthcare AI Company
/@JohnSnowLabs
Jan 13, 2022
This video explores the significant challenges and an AI-powered solution for automating Clinical Trial Master File (TMF) migration and information extraction within pharmaceutical companies. It highlights that TMF migration is a complex, labor-intensive process due to the massive volume of unstructured documents (scanned, handwritten), lack of standardization, and bespoke rules, rendering manual methods and traditional Robotic Process Automation (RPA) ineffective. The presented solution leverages Natural Language Processing (NLP) and Artificial Intelligence, including advanced OCR and machine learning, to classify documents, extract critical metadata, and ensure data accuracy and regulatory compliance. A detailed case study with Novartis demonstrates the real-world application, showcasing substantial reductions in manual effort and migration timelines while adhering to stringent industry standards like GxP and GAMP 5. Key Takeaways: * **TMF Migration Complexity:** Clinical Trial Master File migration is inherently complex due to the lack of content standardization, high volume of unstructured data (scanned, handwritten), and non-explicit, bespoke rules, making manual or basic automation approaches impractical. * **AI-Driven Efficiency & Accuracy:** AI and NLP-based systems, incorporating advanced OCR and machine learning, can achieve an 80% reduction in manual labor and migration timelines for TMFs, significantly improving efficiency and accuracy in metadata extraction and document classification. * **Critical Solution Components:** Successful AI solutions for TMF migration rely on meticulously defined annotation guidelines, sophisticated post-processing rules (which can boost accuracy by 30-40% by handling ambiguities like multiple dates or names), and machine learning-driven false positive detectors to ensure data quality. * **Regulatory Compliance & Enterprise Readiness:** Solutions must be designed for enterprise deployment, offering scalability (e.g., Apache Spark-based), on-premise (air-gapped) security, and rigorous validation for regulatory compliance, including GxP and GAMP 5. * **Collaborative Expertise:** Effective implementation requires a multi-disciplinary team combining deep AI/data science expertise with extensive subject matter knowledge in TMF, document management, IT security, quality, and validation from both the solution provider and the client.

Superior Diabetes Care with 1) Shared Decision Making, 2) a Diabetes Checklist and 3) Screenings
AHealthcareZ - Healthcare Finance Explained
@ahealthcarez
Jan 2, 2022
This video provides an in-depth exploration of three critical systems of care identified by University of Minnesota Medical School researchers that lead to superior diabetes outcomes. Dr. Eric Bricker, from AHealthcareZ, begins by establishing diabetes as a significant "bane of existence" for employee health plans and a major risk factor for severe complications like heart attack, stroke, kidney failure, blindness, neuropathy, and amputations. He emphasizes that given the profound suffering and disability caused by diabetes, any effective treatment strategies should be embraced. The presentation then systematically breaks down each of the three research-backed systems, highlighting their practical application and the pitfalls of neglecting them. The first system discussed is "Shared Decision Making," which advocates for a collaborative dialogue between physician and patient rather than a passive acceptance of doctor's orders. Dr. Bricker stresses the importance of identifying "reasonable management options for the individual," acknowledging the unique circumstances of each patient, such as transportation issues, literacy levels, or access to pharmacies. He provides vivid examples of how pragmatic considerations, often overlooked in rushed seven-minute visits, are essential for effective diabetes management. Without this collaborative approach, he argues, treatment plans are destined to fail. The second system is the implementation of a "Diabetes Care Checklist," drawing a parallel to Dr. Atul Gawande's famous surgery checklist. Dr. Bricker asserts that relying solely on a physician's memory for comprehensive diabetes care is a "horrible approach." He suggests that this checklist, whether written or integrated into an Electronic Medical Record (EMR), should prompt doctors to periodically check crucial metrics like Hemoglobin A1C, ensure annual retina exams by an ophthalmologist, screen urine for protein to detect nephropathy, and monitor kidney function via serum creatinine. He highlights that patients typically present for acute "sick visits," making it the doctor's responsibility, guided by a checklist, to proactively address silent chronic diseases like diabetes that ultimately lead to severe long-term complications. Finally, the third system focuses on "Guideline-Based Screenings" for conditions *outside* of diabetes itself, which are nonetheless crucial for diabetic patients. Dr. Bricker explains that regular screenings recommended by the U.S. Preventive Services Task Force for conditions like hypertension and high cholesterol are vital because these are major risk factors for coronary artery disease, exacerbating the risks already posed by diabetes. He also underscores the importance of screening for depression, as it significantly hinders a patient's ability to self-manage their diabetes. Furthermore, screening for and addressing cigarette smoking and alcohol abuse are critical, as these habits cause immense damage to blood vessels, compounding the vascular issues inherent in diabetes. The video concludes by emphasizing that merely having a primary care physician is not a magical solution; these structured systems of care, including the potential for virtual visits, are essential for improving diabetes outcomes. Key Takeaways: * **Diabetes as a Major Health Burden:** Diabetes is a leading cause of heart attack, stroke, kidney failure, blindness, neuropathy, and amputations, necessitating effective and proactive management strategies to mitigate its severe impact on patient health and healthcare costs. * **Shared Decision Making is Crucial:** Effective diabetes care requires a collaborative dialogue between the physician and patient to identify "reasonable management options" tailored to the individual's unique life circumstances, including social determinants of health like transportation, literacy, and access to resources. * **Individualized Care Over Generic Prescriptions:** A one-size-fits-all approach to diabetes management is ineffective; care plans must be pragmatic and adaptable to the patient's specific challenges to ensure adherence and positive outcomes. * **The Power of a Diabetes Care Checklist:** Implementing a structured checklist, similar to surgical checklists, significantly improves diabetes outcomes by ensuring that essential screenings and interventions are not overlooked, moving beyond reliance on physician memory. * **Essential Diabetes-Specific Screenings:** The checklist should include periodic checks for Hemoglobin A1C (90-day blood sugar control), annual retina exams by an ophthalmologist, urine protein checks for nephropathy, and serum creatinine tests for kidney function. * **Proactive Management of Silent Chronic Diseases:** Physicians must use checklists to proactively address chronic conditions like diabetes during acute "sick visits," as patients rarely initiate discussions about their chronic disease screenings. * **Broader Guideline-Based Screenings are Vital:** Beyond diabetes-specific checks, regular screenings for co-morbidities like hypertension, high cholesterol, depression, cigarette smoking, and alcohol abuse are critical, as these conditions significantly worsen diabetes outcomes and increase overall health risks. * **Addressing Mental Health and Lifestyle Factors:** Screening for and treating depression is paramount, as it severely impairs a diabetic patient's ability to manage their condition. Similarly, addressing smoking cessation and alcohol abuse is crucial due to their damaging effects on blood vessels. * **Structured Care is Not Optional:** Simply having a primary care physician does not guarantee effective diabetes management; superior outcomes depend on the consistent application of structured systems involving shared decision-making, checklists, and comprehensive screenings. * **Virtual Visits Enhance Accessibility:** Especially in contexts like a pandemic, virtual visits offer a highly effective means to implement these three systems of care, improving patient access and adherence to essential diabetes management protocols. Key Concepts: * **Shared Decision Making:** A collaborative process where patients and clinicians make healthcare decisions together, taking into account the best available evidence and the patient's values and preferences. * **Diabetes Care Checklist:** A systematic tool used by healthcare providers to ensure all necessary screenings, tests, and interventions for diabetes management are consistently performed. * **Guideline-Based Screenings:** Preventive health checks and diagnostic tests recommended by authoritative bodies (e.g., U.S. Preventive Services Task Force) for various health conditions, applied to diabetic patients to manage co-morbidities. * **Hemoglobin A1C:** A blood test that measures a person's average blood sugar level over the past 2-3 months, used to monitor diabetes control. * **Nephropathy:** Kidney disease, a common and severe complication of diabetes, often screened for by checking for protein in the urine. * **Serum Creatinine:** A blood test used to measure kidney function. Examples/Case Studies: * **Patient with no transportation:** A patient who could only walk or use public transport, necessitating medication pick-up directly from the clinic rather than a pharmacy. * **Illiterate patient:** A patient who could not read, requiring their spouse to accompany them to appointments to understand instructions. * **Atul Gawande's Surgery Checklist:** Referenced as a successful model for how simple checklists can dramatically improve outcomes in complex medical procedures, applied here to diabetes care.

Best Content for LinkedIN
Self-Funded
@SelfFunded
Dec 27, 2021
This video provides an in-depth exploration of effective content strategies for LinkedIn, based on the speaker's personal experience and data from his 2021 posts. The presenter, Spencer Smith from Self-Funded, shares his analysis of over a year's worth of LinkedIn content, categorizing posts by type and ranking them by average views to identify what resonates most with his professional network. His primary goal for using LinkedIn is for prospecting, sales, and building brand awareness, particularly relevant for individuals and companies in professional services. The speaker immediately challenges the conventional wisdom that LinkedIn should be strictly professional, advocating for the inclusion of personal content. He details seven content categories, presenting them in descending order of average engagement. The top-performing category, "Family," surprisingly garnered the highest average views, demonstrating the power of human connection. This is followed by "Business Insights (Picture)," "Memes," "Podcast Promotional Pics," "Personal Lessons," "Podcast Promotional Clips," and "Business Insights (Video)." He emphasizes that even personal posts should have an underlying professional message or value system, serving as a delivery vehicle for deeper insights. Throughout the analysis, Smith provides specific view counts for his top-performing posts and average views per category, offering concrete data to support his claims. He discusses the nuances of each content type, such as the initial success and subsequent saturation of memes, and the difference in engagement between picture-based business lessons and video-based ones. A key point he highlights is the discrepancy in how LinkedIn counts views for pictures versus videos, noting that videos require a minimum three-second watch time. Despite lower average engagement for his video content, he expresses a commitment to video due to its ability to convey deeper, long-form messages, citing Dr. Eric Bricker of Healthcare Z as an example of someone who successfully leverages video on the platform. The video concludes by stressing the importance of consistency, frequency, and showing up regularly on LinkedIn to exponentially grow one's network and achieve business objectives. Key Takeaways: * **Embrace Personal Content with Purpose:** Contrary to popular belief, personal content, especially family-related posts, can be highly effective on LinkedIn. The speaker's "Family" posts achieved the highest average views (12,700), demonstrating that humanizing your brand and sharing relatable aspects of your life, infused with a professional message, fosters connection and engagement. * **Prioritize Pictures for Business Insights:** While both picture and video formats for business lessons are valuable, the speaker found that picture-based business insights significantly outperformed video, averaging 5,500 views compared to 1,800 for video. This suggests that concise, visually supported text insights are often more digestible for the LinkedIn audience. * **Leverage Memes Strategically:** Memes can be a successful way to communicate professional messages succinctly and engagingly, using culturally relevant templates. However, the speaker noted a drop in engagement over time due to saturation, indicating that this strategy might require freshness and originality to maintain effectiveness. * **Consistency is King for Brand Building:** Regular posting, even if not every post achieves viral status, is crucial for building a consistent presence and brand awareness on LinkedIn. The speaker used his weekly podcast promotions (pictures and clips) as a consistent reason to post, reinforcing his frequency. * **Video Engagement Nuances:** LinkedIn's view count for videos requires a minimum three-second watch time, which can artificially lower reported engagement compared to picture views (which count a millisecond scroll). While the speaker's videos had lower average views, he still advocates for video for its depth and long-form communication potential. * **Personal Lessons Humanize Your Brand:** Similar to family content, sharing personal lessons (e.g., from college, sports) that offer value and are relatable helps humanize your brand and allows your audience to connect with you on a deeper level, fostering trust and rapport. * **LinkedIn as a Free Prospecting and Sales Tool:** The platform offers immense potential for growing a professional network, prospecting, driving sales, and building company awareness, especially for those in professional services. The speaker emphasizes that consistent effort can yield significant results within a year. * **Adapt Content to Platform and Audience:** The speaker's experience highlights that different content types perform differently. While he found videos less engaging for his specific style, he acknowledges others, like Dr. Eric Bricker, who excel with video by honing a particular format (e.g., whiteboard videos). * **Analyze Your Own Data:** The speaker's methodology of reviewing his own 2021 posts and categorizing them by engagement provides a practical framework for others to analyze their content performance and refine their LinkedIn strategy. * **Focus on Underlying Message:** Regardless of the content type (family photo, meme, business lesson), the speaker stresses that every post should have an underlying message or purpose that aligns with your professional brand or value system. Tools/Resources Mentioned: * **LinkedIn:** The primary platform for content strategy discussion. * **YouTube:** Mentioned as a platform for the speaker's podcast. * **Spotify:** Mentioned as a platform for the speaker's podcast. * **iTunes:** Mentioned as a platform for the speaker's podcast. * **Dr. Eric Bricker / Healthcare Z:** Cited as an example of successful video content creator on LinkedIn, known for whiteboard videos on healthcare topics. Key Concepts: * **Content Engagement:** The metric used (views per post) to determine the effectiveness of different content types on LinkedIn. * **Humanization of Brand:** The strategy of sharing personal or relatable content (e.g., family, personal lessons) to make a professional brand more approachable and trustworthy. * **Content Saturation:** The phenomenon where a particular content style (e.g., memes) becomes overused, leading to decreased engagement over time. * **Professional Services:** The target audience for whom the LinkedIn content strategies are particularly relevant, encompassing consulting, advisory, and specialized expertise firms.

Medicare, Medicare Advantage, Part D, Medicare Supplement, Medicaid, Affordable Care Act Explained
AHealthcareZ - Healthcare Finance Explained
@ahealthcarez
Dec 17, 2021
This video provides an in-depth exploration of the major government health insurance programs in the United States, including Traditional Medicare, Medicare Advantage, Medicare Part D, Medicare Supplement plans, Medicaid, and the Affordable Care Act (ACA). Dr. Eric Bricker systematically dissects each program, offering a comparative analysis of their structures, eligibility requirements, coverage benefits, administration, and associated costs. The presentation aims to demystify the complex landscape of healthcare finance for a broad audience, including professionals in the pharmaceutical and medical device industries who need to understand the payer environment. The discussion begins with Medicare, detailing its traditional form (Parts A and B) for individuals 65 and older, highlighting its low premiums but significant out-of-pocket costs like deductibles and the 20% Part B co-insurance with no out-of-pocket maximum. Traditional Medicare, administered by the Centers for Medicare & Medicaid Services (CMS), offers greater freedom in provider choice and does not require prior authorizations or referrals. In contrast, Medicare Advantage (Part C), administered by private commercial insurance companies like UnitedHealthcare and Humana, combines A and B coverage, often includes additional benefits such as dental, vision, and hearing, and prescription drug coverage. While Medicare Advantage plans often have low or zero premiums, they typically operate as HMOs or narrow network PPOs, limiting provider choice and requiring referrals and prior authorizations. The video emphasizes the significant profitability of Medicare Advantage for private insurers, who receive approximately $1,000 per beneficiary per month from the government. The video then moves to Medicare Part D, which provides prescription drug coverage for those on Traditional Medicare, administered by private Pharmacy Benefit Managers (PBMs) of health insurance companies. It explains the tiered formulary structure, co-pays, and the controversial "donut hole" gap in coverage, which was designed for funding purposes but can be eliminated by some plans. Medicare Supplement plans (Medigap) are introduced as additional private insurance to cover the out-of-pocket expenses not covered by Traditional Medicare Parts A and B, such as deductibles and co-insurance. Following Medicare, the discussion shifts to Medicaid, a state-administered program for low-income individuals under 65, jointly funded by federal and state governments. Medicaid plans are almost exclusively HMOs, managed by large commercial insurers like Centene and Molina, and impose significant restrictions on provider choice and require referrals and prior authorizations. Finally, the Affordable Care Act (ACA) is explained as a federal initiative to expand health insurance coverage to the uninsured, particularly those earning between 125% and 400% of the federal poverty level who do not receive employer-sponsored insurance. ACA plans, purchased through state or federal exchanges (e.g., Healthcare.gov), are heavily subsidized by the government, must offer "minimal essential coverage," but often come with high deductibles and co-insurance. A notable challenge, the "family glitch," is highlighted, where individuals offered employer coverage for themselves but not their families are ineligible for ACA subsidies for their dependents. Key Takeaways: * **Diverse Government Programs:** The U.S. healthcare system is heavily influenced by a variety of government-backed insurance programs, each with distinct structures, eligibility, and coverage rules, impacting patient access to care and medications. * **Traditional Medicare vs. Medicare Advantage:** Seniors turning 65 have a choice between Traditional Medicare (Parts A & B), offering broad provider choice but higher out-of-pocket costs, and Medicare Advantage (Part C), which typically has lower premiums, includes more benefits (dental, vision, prescriptions), but restricts provider networks and requires referrals. * **Private Insurer Dominance:** Private commercial insurance companies (e.g., UnitedHealthcare, Humana, Aetna, Centene, Molina) play a significant role in administering various government programs, including Medicare Advantage, Medicare Part D, Medicaid, and ACA exchange plans, acting as intermediaries between the government and healthcare providers. * **Profitability of Medicare Advantage:** Medicare Advantage plans are highly profitable for private insurers, with the government paying approximately $1,000 per beneficiary per month, making it a lucrative segment for health insurance companies. * **Prescription Drug Coverage (Part D):** Medicare Part D provides essential prescription drug coverage for Traditional Medicare beneficiaries, administered by private PBMs, and features tiered formularies and the "donut hole" coverage gap, which some plans may eliminate. * **Medicare Supplement Plans (Medigap):** These private plans are crucial for Traditional Medicare beneficiaries seeking to cover the significant out-of-pocket expenses (deductibles, co-insurance) not fully covered by Parts A and B. * **State-Administered Medicaid:** Medicaid is a state-level program for low-income individuals, with rules varying by state, and is predominantly administered through commercial HMO plans, leading to restricted provider access and requiring gatekeepers and prior authorizations. * **ACA's Role in Expanding Coverage:** The Affordable Care Act significantly expanded health insurance coverage to millions of previously uninsured individuals by providing subsidized plans through exchanges for those above Medicaid eligibility but without employer-sponsored insurance. * **ACA Challenges: High Deductibles and "Family Glitch":** Despite subsidies, ACA plans often feature high deductibles (e.g., $2,000-$6,000), functionally leaving some insured individuals with significant financial barriers to care. The "family glitch" prevents families from receiving ACA subsidies if one member is offered employer coverage, even if family coverage is unaffordable. * **Impact on Commercial Operations:** Pharmaceutical and life sciences companies must deeply understand these payer dynamics, especially Medicare Part D and the varying coverage models, to effectively strategize market access, pricing, and commercial operations for their products. * **Regulatory Compliance Context:** While not directly discussed, the complex interplay of government programs and private administration creates a challenging regulatory environment that companies must navigate for market access and patient support programs. **Key Concepts:** * **Traditional Medicare (Parts A & B):** Federal health insurance for seniors (65+) and certain younger people with disabilities. Part A covers hospital services; Part B covers doctor and outpatient services. * **Medicare Advantage (Part C):** An alternative to Traditional Medicare, offered by private insurance companies approved by Medicare, often including additional benefits and prescription drug coverage. * **Medicare Part D:** Prescription drug coverage for Traditional Medicare beneficiaries, administered by private insurance companies/PBMs. * **Medicare Supplement Plans (Medigap):** Private insurance plans that help pay for out-of-pocket costs not covered by Traditional Medicare. * **Medicaid:** A joint federal and state program that helps with medical costs for some people with limited income and resources. * **Affordable Care Act (ACA) / Obamacare:** Federal legislation passed in 2010 aimed at reforming the healthcare system, expanding insurance coverage, and regulating health insurance companies. * **CMS (Centers for Medicare & Medicaid Services):** The federal agency that administers Medicare, Medicaid, and the Children's Health Insurance Program (CHIP). * **PBMs (Pharmacy Benefit Managers):** Third-party administrators of prescription drug programs for commercial health plans, self-insured employer plans, Medicare Part D plans, and government programs. * **HMO (Health Maintenance Organization):** A type of health insurance plan that usually limits coverage to care from doctors who work for or contract with the HMO, often requiring a primary care physician (PCP) gatekeeper and referrals. * **PPO (Preferred Provider Organization):** A type of health insurance plan where you pay less if you use doctors, hospitals, and providers that belong to the plan's network. * **Federal Poverty Level (FPL):** A measure of income issued annually by the Department of Health and Human Services, used to determine eligibility for many federal programs and benefits. * **Donut Hole (Coverage Gap):** A temporary limit on what the Medicare Part D drug plan will cover for prescription drugs, where beneficiaries pay a higher percentage of drug costs until they reach a certain out-of-pocket spending threshold. * **Minimal Essential Coverage:** The type of health coverage an individual must have under the ACA to avoid a penalty (though the penalty was later eliminated). * **Actuarial Value:** The percentage of average healthcare costs that a health insurance plan will cover. * **Family Glitch:** A loophole in the ACA that prevents families from receiving subsidized health insurance through the exchanges if one family member is offered "affordable" employer-sponsored coverage, even if the family coverage itself is unaffordable. * **Prior Authorization:** A requirement from your health insurance company that your doctor obtain approval before you can get a specific service or medication. * **Referrals:** An order from your primary care doctor for you to see a specialist or get certain medical services. **Examples/Case Studies:** * **Medicare Advantage Growth:** The video notes the rapid growth of Medicare Advantage plans, from 20% to 40% of seniors in just a few years, indicating a significant shift in the senior insurance market. * **Major Private Insurers:** Specific companies like UnitedHealthcare, Humana, Aetna, Cigna, Anthem, Centene, Molena, and Oscar are mentioned as key players in administering various government health insurance programs. * **State-Specific Medicaid Examples:** Illinois (Meridian, Family Health Network, Harmony) and New York (16 different options including Blue Cross Blue Shield, UnitedHealthcare, Molena) are cited to illustrate the state-level administration and varied plan options for Medicaid. * **ACA Exchange Websites:** Healthcare.gov is mentioned as the federal exchange, while states like California run their own state-specific ACA websites. * **The "Family Glitch" Scenario:** A concrete example of a breadwinner making $50,000 a year, offered individual employer coverage but unable to afford family coverage, and thus ineligible for ACA subsidies for their family, is used to explain the "family glitch."

How Prescription Drug Coverage Works: Formulary Tiers, PBM, Rebates, Spread-Pricing Explained
AHealthcareZ - Healthcare Finance Explained
@ahealthcarez
Dec 11, 2021
This video provides an in-depth exploration of how prescription drug coverage functions within the U.S. healthcare system, focusing on formularies, formulary tiers, and the intricate financial mechanisms of Pharmacy Benefit Managers (PBMs). The presenter, Dr. Bricker, begins by establishing the significant impact of prescriptions, noting they constitute approximately 20% of all healthcare spending, thus necessitating a clear understanding of their coverage. The discussion progresses from the foundational concept of a formulary—a list of covered medications—to the nuances of non-formulary drugs and the tiered structure that dictates patient co-pays. The core of the video delves into the role and operations of Pharmacy Benefit Managers (PBMs), which are presented as critical intermediaries, often divisions of major health insurance companies. PBMs are responsible for negotiating drug prices with pharmaceutical manufacturers, determining which drugs are included in formularies, and assigning them to specific tiers. The video identifies the four major PBMs—Express Scripts (now Evernorth/Cigna), Caremark (CVS Health/Aetna), OptumRx (UnitedHealth Group), and Prime Therapeutics (Blue Cross plans)—highlighting their dominant market share and their integration within larger healthcare conglomerates. A significant portion of the analysis is dedicated to demystifying how PBMs generate revenue, explaining two primary methods: rebates and spread pricing. Rebates, applied to brand-name medications, are depicted as commissions paid by pharmaceutical manufacturers to PBMs, a substantial portion of which PBMs retain, passing only a fraction to employers as a "rebate." This system, the speaker argues, creates an incentive for PBMs to favor higher-cost drugs and increased prescription volume. Spread pricing, conversely, applies to generic medications, where PBMs purchase drugs at a low cost but charge employers a significantly higher, marked-up price, often based on a fictitious "Average Wholesale Price" (AWP), creating a substantial profit margin for the PBM. Key Takeaways: * **Prescription Drug Spending:** Prescriptions account for a substantial 20% of total healthcare spending, underscoring the importance of understanding their coverage and cost structures. * **Formulary and Non-Formulary Medications:** A formulary is a list of medications covered by insurance, while non-formulary drugs (e.g., most over-the-counter, cosmetic, and some reproductive medications) are typically not covered, requiring patients to pay cash. * **Tiered Formulary Structure:** Health plans typically categorize covered medications into four tiers—Generics (Tier 1, lowest co-pay), Preferred Brand (Tier 2), Non-Preferred Brand (Tier 3, higher co-pay), and Specialty Medications (Tier 4, highest cost, often 20% coinsurance). These tiers directly influence patient out-of-pocket costs. * **High Cost of Specialty Medications:** Specialty drugs are exceptionally expensive, often costing thousands of dollars per month, and are typically used for complex conditions like rheumatoid arthritis, HIV, or hepatitis C. Their high cost, combined with coinsurance, can lead to significant annual patient expenses. * **Role of Pharmacy Benefit Managers (PBMs):** PBMs are crucial intermediaries that negotiate drug prices with pharmaceutical manufacturers, establish formularies and tiers, and process pharmacy claims. They are predominantly owned by major health insurance companies, creating integrated healthcare ecosystems. * **PBM Revenue through Rebates:** For brand-name drugs, PBMs receive "rebates" (effectively commissions) from pharmaceutical manufacturers. PBMs often retain a large portion of these rebates, passing only a smaller percentage to employer clients, which incentivizes PBMs to favor higher-cost medications and increased prescription volume. * **PBM Revenue through Spread Pricing:** For generic medications, PBMs profit from "spread pricing," where they charge employer clients a significantly higher price than what they reimburse pharmacies for the drug. This spread can be substantial, often based on an inflated "Average Wholesale Price" (AWP) that is not reflective of actual acquisition costs. * **Fictitious Pricing Benchmarks:** The "Average Wholesale Price" (AWP) used in generic drug pricing is often a made-up figure, leading to a lack of transparency and enabling PBMs to negotiate discounts off an artificially high starting point, further obscuring the true cost and profit margins. * **Self-Funded Plan Flexibility:** Employers with self-funded health plans have the option to "carve out" their PBM services, allowing them to choose an independent PBM or one from a competing health insurance carrier, potentially offering more flexibility and cost control. * **Patient Cost-Saving Strategies:** Patients should be aware that the cash price of some generic medications can be lower than their insurance co-pay. Tools like GoodRx can help patients compare prices and potentially save money by paying cash instead of using insurance. * **Clinical Efficacy vs. Cost:** For certain conditions, highly effective and significantly cheaper generic first-line therapies (e.g., methotrexate for rheumatoid arthritis) exist, yet patients are often prescribed expensive specialty drugs (e.g., Humira) without first trying the generic option, leading to higher costs for both patients and health plans. **Key Concepts:** * **Formulary:** A list of prescription drugs covered by a health insurance plan. * **Non-Formulary:** Medications not covered by a health insurance plan. * **Formulary Tiers:** Categories of drugs within a formulary, each with a different co-payment or coinsurance level. * **Co-pay:** A fixed amount a patient pays for a covered healthcare service, including prescriptions, after their deductible has been met. * **Coinsurance:** A percentage of the cost of a covered healthcare service that a patient pays after their deductible has been met. * **Pharmacy Benefit Manager (PBM):** A third-party administrator of prescription drug programs for health insurance companies, Medicare Part D plans, and large employers. * **Rebates:** Payments from pharmaceutical manufacturers to PBMs, often tied to formulary placement or market share, which PBMs may partially pass on to clients. * **Spread Pricing:** The practice where a PBM charges a health plan or employer more for a drug than it reimburses the pharmacy for dispensing it, keeping the difference. * **Average Wholesale Price (AWP):** A benchmark price for prescription drugs, often considered an inflated list price that is not reflective of actual transaction prices. * **Maximum Allowable Cost (MAC):** The maximum amount a PBM will reimburse a pharmacy for a generic drug. * **National Average Drug Acquisition Cost (NADAC):** A survey-based measure of the actual cost pharmacies pay to acquire prescription drugs. * **Self-Funded Plan:** An employer-sponsored health plan where the employer directly pays for employees' healthcare costs rather than paying premiums to an insurance carrier. * **Carve Out PBM:** The practice by self-funded employers of contracting directly with a PBM separate from their medical insurance carrier. **Tools/Resources Mentioned:** * **GoodRx:** A platform mentioned as a resource for patients to check cash prices for medications, potentially finding lower costs than their insurance co-pay. **Examples/Case Studies:** * **Non-Formulary Medications:** Tylenol (OTC), cosmetic creams for wrinkles, Viagra (lifestyle medication), and certain infertility treatments are cited as examples of drugs typically not covered by insurance. * **Formulary Tiers:** The cholesterol medications Simvastatin (generic), Zocor (preferred brand), and Crestor (non-preferred brand) are used to illustrate how different tiers lead to varying co-pays ($10, $30, $60 respectively). * **Specialty Medications:** Humira (for rheumatoid arthritis and Crohn's disease), certain HIV pill medications, oral chemotherapies, and Hepatitis C treatments (e.g., a $40,000 one-month supply) are highlighted as examples of extremely expensive specialty drugs. * **Cost-Saving Alternative:** Methotrexate, a generic medication, is presented as an effective and significantly cheaper first-line therapy for rheumatoid arthritis compared to Humira, emphasizing the potential for substantial cost savings if patients are started on appropriate generic alternatives. * **Cash Price vs. Co-pay:** A personal anecdote about a diaper rash cream costing $1.80 cash versus a $10 co-pay demonstrates how paying cash can sometimes be more economical than using insurance for low-cost generics.